Reactive epithelial changes are dangerous for women's health. And at the same time, they rarely manifest themselves somehow. The asymptomatic course at times complicates the diagnosis. Therefore, all women are recommended to contact the gynecological office at least once a year to conduct a cytological examination of microflora.
Why do these changes occur at all? What are the prerequisites and reasons? Are there any symptoms? This and much more will now be discussed.
Norm indicators
First you need to talk about them. The uterus consists of three layers - the internal mucosa (also called endometrium), muscle and integumentary.
Normally, the surface of her neck is pink and smooth. This is due to the uniform layer of the basal epithelium. Normally, the Schiller test indicator (diagnostic measure) turns brown.
During the cytological analysis, a single number of leukocytes, as well as flat epithelial cells, should be detected on the studied fragment.
White blood cells are normally characterized by whole nuclei and pure cytoplasm. There are no signs of phagocytosis. In smears, cells with transformed cytoplasm and mucus can be found.

Pathogenesis
Reactive changes in the epithelium occur due to infection of a woman with an infection. This happens, as a rule, due to unprotected intercourse with an unverified partner.
About 50% of all infections differ in the bacterial nature of origin. Inflammation of the vaginal membranes provokes a similar process that occurs in the cervix.
Interestingly, in some cases, even the bacteria that make up the natural microflora of the genital tract are infectious agents. But this happens only under the condition of weakened immunity.
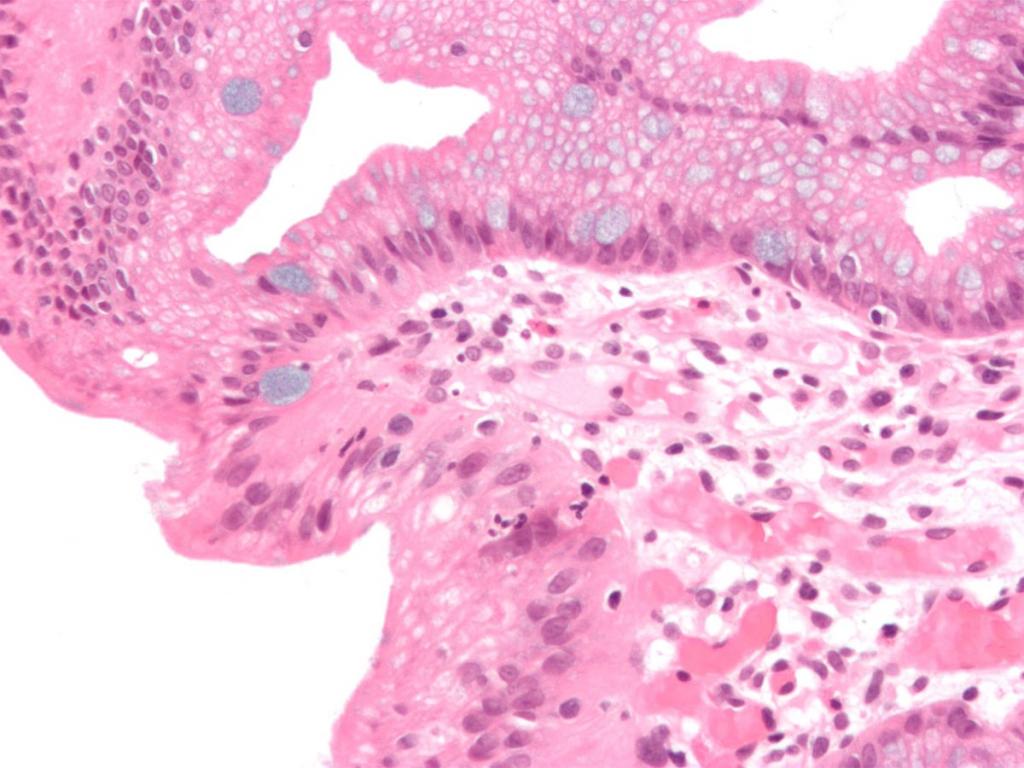
An initial examination aimed at detecting reactive changes in the epithelium reveals inflammation. Analysis for cytology shows the content of a large number of white blood cells with destroyed nuclei, eosinophilic and lymphoid elements. If we talk about microflora, then with reactive changes in the epithelium, it becomes mixed.
If the inflammation is detected on time, then it can be successfully overcome with the help of adequate antibacterial treatment. Therapy is completed by the restoration of microflora - prebiotics are used for this.

Classification
After a cytological analysis, the following reactive changes in squamous epithelium are revealed:
- Exudative. In a woman, destroyed neutrophilic white blood cells are detected . The smear contains fragments of cells and nuclei. The surviving, whole, are in a state of phagocytosis.
- Reparative. The name for this type of change was given to the repair and subsequent epithelization taking place in the defective surface of the layers. According to the results of the analysis, cells of increased sizes are detected. It is because of them that tissue grows, which replenishes the affected areas. Nuclei become larger, but do not lose clear contours. Chromatin conglomeration is not observed. Incidentally, it is distinguished by a delicate-granular structure.
- Degenerative Manifested by wrinkling of the cell nucleus. Violations of the structure of the nuclear membrane and chromatin are also observed. A chronic inflammatory process is indicated by the proliferation of the epithelium.
Talking about reactive changes in squamous epithelium, it is necessary to make a reservation that cytological analysis also often reveals a combination of inflammatory changes. Often, reparative are combined with degenerative and proliferative.
In such cases, multinucleated cells with large nuclei are detected. The cytological picture strongly resembles dysplasia or cancerous conditions. If we talk about inflammatory atypia, then it is characterized by a uniform distribution of chromatin. Blocks have fuzzy contours.
Proliferation
So called reactive changes in the glandular epithelium. How is it manifested? An increase in the number of cellular glandular components localized in the cervical canal. This is not an independent disease, but a complex of cytological changes.
So, moderate proliferation indicates pseudo-erosion. During the examination, it is possible to detect signs of the disease in the vaginal segment, where they are absent normally. As part of the diagnosis, a visual examination, smear cytology and colposcopy are performed.
If a woman develops inflammation, accompanied by proliferation, then she may feel pain in the vagina and discomfort. When the cause is hormonal imbalance, then there are also bloody discharge between menstruation, amenorrhea and other symptoms.
The cause is not always trauma or infection. Even in a healthy woman, proliferation can occur if she takes OK and often neglects pharmaceutical rules.
The treatment that the doctor prescribes is always aimed at eliminating the reason why this ailment appeared. If, for example, it arose due to an infection, then antibacterial therapy will be effective.
Erosion
So, what is meant by "reactive changes in the epithelium" is clear. Now we should delve into the study of this topic and consider specific diseases.
Cervical erosion is a defect consisting in damage to the notorious squamous epithelium around the external pharynx.
Of course, the cause is the inflammatory process. Erosion occurs in most women who have had cervicitis and endocervicitis. Although there is still a version according to which the reason is a change in the level of steroid sex hormones. There is some truth to this, as clinical observations have helped to identify symptoms of erosion during pregnancy. In the postpartum period, they pass, since the hormonal background is stabilized.
Erosion is characterized by a relapsing, prolonged, persistent course. This disease is not amenable to conservative therapy. But unfortunately, the diagnosis is difficult, since there are no characteristic complaints in women. In addition, this ailment, which leads to reactive changes in the epithelial cells, is also asymptomatic.
Pathology can be detected during a visual examination of the cervix, as well as through colposcopy.
Erosion treatment
The basis of therapy aimed at eliminating this disease is a mechanism aimed at the destruction of the cells of the cylindrical epithelium. The goal is their rejection and the further restoration of squamous epithelium.
There are several methods that help to achieve the result:
- Diathermocoagulation. During the procedure, the altered tissue is cauterized with an alternating high-frequency electric current. It provokes tissue heating, due to which the desired effect arises. This procedure is contraindicated for nulliparous patients, since scars form as a result, and they prevent the cervix from opening at the time of delivery. Also, the method is traumatic. Healing lasts approximately 1.5-3 months. Often endometriosis becomes a consequence, so it is advisable to carry out the procedure in the second phase of the menstrual cycle.
- Laser vaporization. This is a "cauterization" of laser erosion. Ideally, it should be carried out on the 5-7th day of the cycle. Sanitation of the cervix and vagina is preliminarily prescribed. The whole procedure is painless, does not leave scars. Full regeneration is observed after a month.
- Radio wave treatment. During this procedure, a high frequency electromagnetic wave acts on the pathological focus. Physically they cannot be felt. The procedure takes less than a minute, and anesthesia and treatment in the postoperative period are not required.
- Cryodestruction. It implies freezing of erosion tissues with liquid nitrogen or its nitrous oxide. The procedure is fraught with neither pain, nor blood, nor scars. During the first day, the patient will experience abundant liquid discharge and swelling. But it will pass quickly. It takes one to one and a half months to heal.
It should be noted that any of the listed procedures is prescribed only after a detailed diagnosis of reactive changes in epithelial cells.
It is important to carry out all the procedures - starting with targeted biopsy, ending with colposcopy to exclude the oncological process. If the doctor reveals the prospect of malignant transformation, then the patient will be prescribed surgery.

Leukoplakia
Continuing to talk about reactive changes in the cervical epithelium, it is necessary to raise attention to this disease.
What is it like? Leukoplakia is a pathological change in exocervix, which is characterized by proliferation and keratinization of the stratified epithelium.
The cause may be traumatic, chemical or infectious effects, as well as the influence of endogenous factors (impaired immune and hormonal regulation). A violation of the functional relationship between the uterus, ovary, pituitary and hypothalamus also plays a role. Because it is fraught with anovulation, hyperextrogenia and progesterone deficiency.
Predisposing factors are promiscuous sexual intercourse and a woman’s disease. Squamous cells with reactive changes are observed in patients suffering from one of the following:
- Adnexitis.
- Endometritis.
- Oligomenorrhea or amenorrhea.
- Chlamydia
- Ureaplasmosis.
- Herpes.
- Mycoplasmosis
- Cervicitis.
- Colpitis.
- Ectopia.
Usually this ailment is asymptomatic, but sometimes accompanied by contact secretions and leucorrhoea. Diagnostic principles are the same as in the case of erosion. Additionally, scrapings and a biopsy are examined, which are taken for histological examination of the material.
Treatment of this reactive change in the cervical epithelium is aimed at eliminating background diseases, as well as at the complete removal of foci where the pathology has manifested itself. According to the doctor’s testimony, antiviral, antibacterial and anti-inflammatory therapy is performed. Still often resort to one of the procedures shown during erosion (described above).

Erythroplakia
Studying the conditions in which squamous cells with reactive changes are observed, it is necessary to talk about this disease. Erythroplakia is a precancerous pathological condition in which the exocervix mucosa atrophies.
It is also asymptomatic. Mucous discharge and bleeding are sometimes observed. The causes of occurrence are the same as in previous cases, but burdened heredity may still occur. Scientists have not yet been able to prove the presence of erythroplakia with chromosomal and gene aberrations. However, according to statistics, the likelihood of the formation of an ailment is much higher in those girls in whose family it has already occurred in women.
By the way, trauma can also be the cause of inflammation with reactive changes in the epithelium. Rupture of the cervix often occurs during childbirth, gyroscopy, abortion and curettage.
With erythroplakia, all natural processes of renewal, as well as the maturation and further rejection of exocervix cells, are disrupted. This leads to an imbalance between the cells of several layers of the membrane at once. Over time, the vaginal mucosa becomes thinner.
The disease is asymptomatic, only severe, advanced cases are accompanied by bleeding.
If squamous cells with reactive changes are detected, and it turns out that this led to erythroplakia, surgical treatment is prescribed. Conservative therapy is pointless. Either minimally invasive intervention or cervical conization is indicated.
Cervical dysplasia
With this ailment, a cytogram with reactive changes in the epithelium demonstrates the formation of atypical cells in those places where a single-layer mates with a multi-layer.
It develops in three stages. At the last stage, a cylindrical epithelium with reactive changes of such a serious nature is observed that in the end it leads to cervical cancer.
This condition occurs initially due to the herpes virus or HPV. Provoking factors include:
- Severe, prolonged diseases of a chronic nature.
- Early sexual life and childbirth at a young age.
- Active or passive tobacco abuse.
- Immunodeficiency.
- Hormonal disorders resulting from pregnancy, menopause or abuse of hormonal drugs.
- Cervical injuries.
Talking about the reactive changes in the cells of the cylindrical epithelium and other aspects of the topic under discussion, it should be noted that dysplasia does not have an independent clinical picture. It proceeds secretly in about 10% of women. But often a microbial infection joins, each of which almost always makes itself known. In many cases, this is gonorrhea, condylomas, chlamydia.
As part of the diagnosis, a cervical examination, a cytological examination of a PAP smear, colposcopy, a biopsy study are performed, and they also resort to immunological PCR methods.
What about treatment? With extensive lesions, the use of interferons and their inducers, as well as immunomodulators, is indicated. In severe cases, surgical intervention is indicated - either the dysplasia zone or the entire cervix is removed.

Cervical Canal Polyps
Much has been said above about reactive changes in the squamous and cylindrical epithelium. There is another pathological condition - it is characterized by the formation of polyps in the cervical canal.
These are tumor-like formations that come from the cylindrical epithelium. They grow directly into the lumen.
This pathology is mainly encountered by women over 40 years old. It is believed that the cause is age-related changes, hormonal disorders, problems with the immune system, stress. Predisposing factors are mechanical injury, diagnostic curettage, endocercivitis of a chronic nature.
In approximately 75% of cases, polyps are combined with erosion, myoma, ovarian cyst, atrophic colpitis, pseudo-erosion. Still at risk are women who have candidiasis, herpes, mycoplasmosis, ureaplasmosis, trichomoniasis, HPV, etc.
The course is asymptomatic. Polyps are detected visually. Diagnosis is performed by colposcopy, cervical biopsy, ultrasound.
Any polyp is an indication for its removal. After this procedure, curettage is carried out so that the leg does not remain inside. The polyp bed is additionally treated with a radio frequency or cryogenic method. When identifying echographic signs, hysteroscopy is indicated. Then, curettage of the uterine cavity is also performed.
Flat cervical papilloma
This neoplasm is very dangerous, since it is quite capable of provoking the development of cancer. It all starts with the penetration of HPV into the body. The virus infects the cells of the mucous membrane and skin, due to which the tissues begin to grow.
Provoking factors include:
- Alcohol abuse.
- Pregnancy.
- Reception of cytostatics.
- Smoking.
- Vitamin deficiency.
- Earlier onset of sexual activity.
- Atopic dermatitis.
- Papilloma removal.
- Disturbed microflora in the vaginal cavity and in the intestine.
- Local manifestations of the disease.
Symptoms may not be for a long time. Flat papilloma can be detected during the examination, during the aforementioned diagnostic measures.
Symptoms appear only when the neoplasm has reached a large size. A woman begins to feel a burning sensation in the genital area, her inguinal lymph nodes increase, and a specific mucus begins to stand out from the vagina.
After the detection of papilloma, it is necessary to begin medication. Doctors often prescribe Gardasil. It is important to combine it with taking drugs that increase the body's defenses. As a rule, it is recommended to use such funds:
- Immunomodulators - "Interferon" or "Genferon".
- Cytostatics - 5-fluorouracil, Bleomycin and Podophyllin.
- Antiviral - Panavir and Isoprinosine.
Destructive drugs can also be prescribed, the use of which helps to destroy the growths. But in severe cases, of course, surgical treatment is prescribed.

Prevention
Each girl is recommended at least once a year to undergo an examination with a gynecologist. Based on the foregoing, it was possible to understand that many serious ailments can be asymptomatic, and when they make themselves felt, it will be too late for conservative therapy.
Treatment is also always prescribed individually. The origin of the inflammation, the age of the patient, whether she plans a pregnancy and, of course, the type of pathology are taken into account.
But the most important thing is a responsible approach to choosing sexual partners. There may not be a permanent man, but protection is always necessary. Because it is STDs that lead to reactive changes.
And you also need to constantly maintain your immunity, regularly strengthen it. Because the weakened defenses of the body provide the best conditions for the development of the virus.
And of course, it is necessary to carefully select oral contraceptives. The doctor is engaged in their selection. The wrong choice of pills can be fraught with serious consequences. A disturbed hormonal background is one of the causes of reactive changes.