Bionic eye - myths and reality
Can you imagine what a person feels who does not see or almost does not see the world around? This condition is called blindness - the inability to perceive visual stimuli due to pathological disorders in the eye itself, in the optic nerves or in the brain. In 1972, the World Health Organization (WHO) adopted the following definition: a person is considered blind if the sharpness of central vision in conditions of maximum correction does not exceed 3/60. With this vision, a person in daylight conditions with maximum optics correction is unable to count fingers from a distance of 3 meters.
So for such cases, the idea of electrical stimulation of the retina or visual cortex was proposed, the creation of a prosthesis that, by the mechanism of action, simulates the actual processes of transmission of electrical signals.
There are several variants of electronic implants; every year new ideas appear, but the term and the Bionic Eye itself were developed by Daniel Palanker, a staff member at Stanford University and his scientific group Biomedical Physics and Ophthalmic Technologies.
The implantation of the Argus II bionic eye model (by the way, the only model that has an EU brand, but not certified in Russia) was performed in Russia in July 2017 for one patient. And from all sources of television broadcasting we heard - now a person will be able to see the world as before. Hundreds of people are asked to put a bionic eye, and some also ask to “implant” the chips for super viewing.
So what do we have today and can a dream come true to see the world after having lost sight?
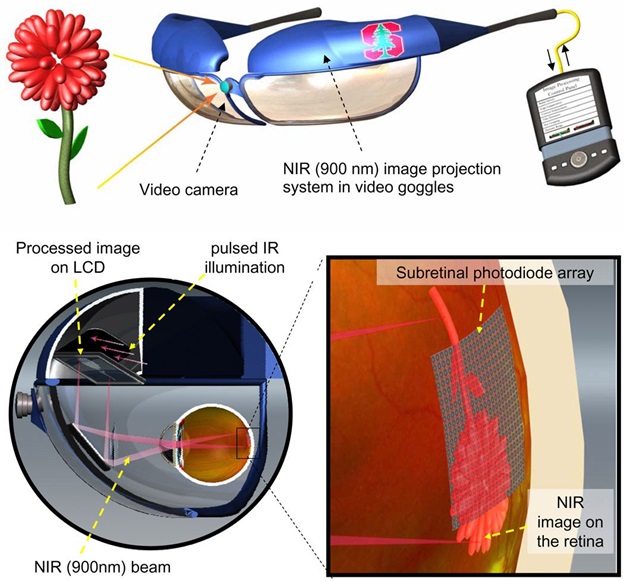
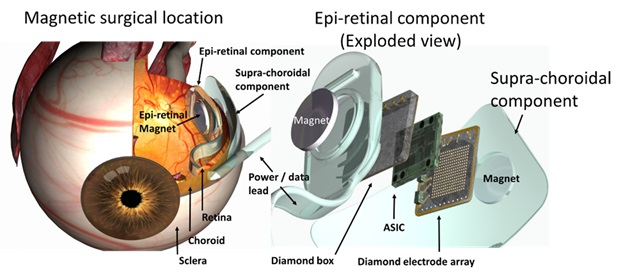
Bionic are called artificial limbs and implantable elements of parts of the human body that are similar in appearance and function to real organs or limbs. Today, bionic arms, legs, hearts, and also organs of hearing successfully help people to have a full life. The purpose of the electronic eye is to help the visually impaired with problems of the retina or optic nerve. Implantable instead of the damaged retina, the device should replace millions of photoreceptor cells of the eye, if not 100%.
Eye technology is similar to that used in hearing aids that help deaf people to hear. Thanks to her, patients are less likely to lose their residual vision, and those who lose their sight see the light and have at least some ability to orient themselves in space.

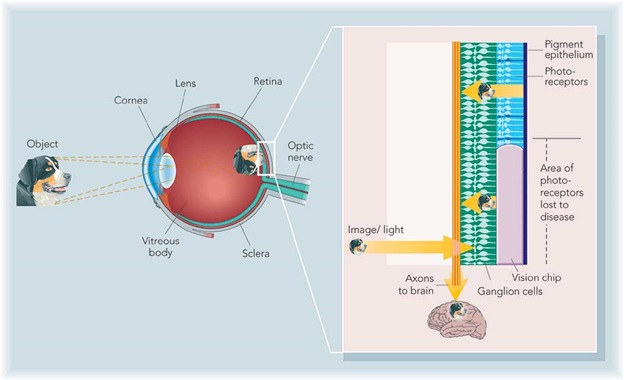
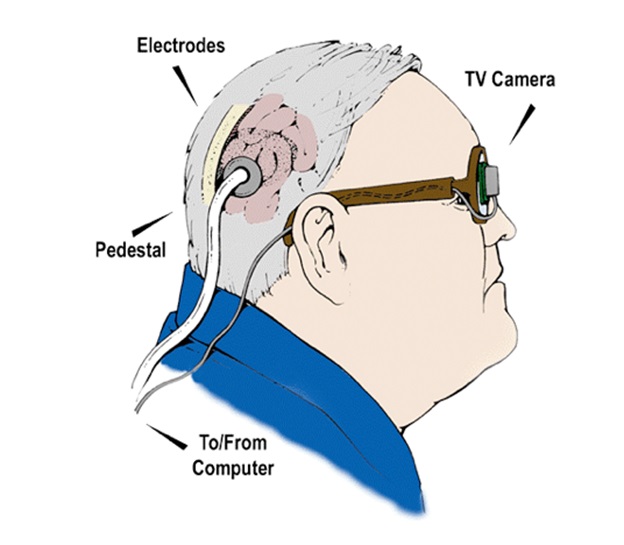
The general principle of the electronic eye is as follows: a miniature camera is embedded in special glasses, information about the image is transmitted to the device, which converts the image into an electronic signal and sends it to a special transmitter, which in turn sends an electronic signal to an implanted eye or brain the receiver, or information is transmitted through tiny wires to the electrodes attached to the retina, they stimulate the remaining nerves of the retina by sending electrical impulses to the brain cut optic nerves. The device is designed to compensate for lost visual sensations with complete or incomplete loss of vision.
The main conditions for successful operation of the system:
These are the most extensive operations. If you describe, for example, the implantation of a subretinal (located under the retina) bionic eye, you need to fully lift the retina, then do an extensive retinectomy (cut off part of the retina), then install this chip under the retina, then retina the retina with a retinal laser, glue the retina with laser coagulation and pour silicone oil . Silicone tamponade is necessary, otherwise PVR (proliferative vitreoretinopathy) will immediately appear and detachment will occur. Yes, there should be no own lens, or it should be replaced with an artificial lens beforehand.
For the operation you need special tools with gentle silicone tips. This is a completely complicated operation, moreover, an orofacial surgeon or an ENT is still needed - they bring the electrodes out through the skin. And it turns out such a device - a chip inside the eye, and in the hands of such a device the size of a mobile phone, with which you can change the signal intensity, it connects to the subcutaneous electrodes. One ophthalmologist-surgeon during the operation is not enough - help from other disciplines is needed, the operation lasts a long 6 hours.
1. The results are quite modest - after the operation, such people cannot be called sighted, they see a maximum of 0.05, i.e. they can see the contours and determine the direction of movement of the shadow, do not distinguish colors at all, objects can only differ from those that are remembered from the former "sighted" life, for example: "aha - this is probably a banana, because something is semicircular." They see that something is moving on them, they can guess that this is a man, but his face is not distinguished.
2. Under what diseases can a bionic eye be useful?
The first patients are patients with retinitis pigmentosa (retinitis pigmentoza), a disease with a primary disappearance of photoreceptors and secondary atrophy of the optic nerve. In Russia, there are 20-30 thousand such patients, in Germany only a few thousand.
Next in line are patients with geographic atrophic macular degeneration. This is an extremely common age pathology of the eye.
The third will be patients with glaucoma. Glaucoma has not yet been studied, since the atrophy of the optic nerve in this case is primary, so the mode of transmission must be different - bypassing the optic nerve.
Diabetes is the most difficult problem to solve. One of the methods of treating diabetic changes on the retina is laser coagulation over the entire surface. After such a procedure, it is technically impossible to lift the retina due to coagulants - this results in a “sieve”. And if it is not made by a laser, the situation is no better: usually the eye is so damaged that implantation is useless in this case.
3. Unfortunately, the current prototype of the bionic eye does not allow people to see the world around us as we see it. Their goal is to move independently without assistance. Until the mass use of this technology is far, however, scientists will give hope to people who have lost their sight.
In the past few decades, scientists from different countries have been working on the ideas of bionic electronic eyes. Each time, technologies are improving, but no one has yet introduced their product to the market for mass use.
The Argus retinal prosthesis is an American project that is fairly well commercialized. The first model was developed by a team of researchers in the early 1990s: Pakistani-born ophthalmologist Mark Hameiun (Mark Humayun, by the way, Professor Sekundo is familiar with him from Johns Hopkins University - at that time he was a resident of the 2nd year, Walter was a student) Eugen Dayan, engineer Howard Phillips, bioengineer Ventay Lew and Robert Greenberg. The first model, released in the late 1990s, by Second Sight had only 16 electrodes.
The “field trials” of the first version of the bionic retina were carried out by Mark Hameiun in six patients with vision loss as a result of retinitis pigmentosa disease in the period from 2002 to 2004. Retinitis pigmentosa is an incurable disease in which a person loses sight. It is observed in approximately one case for every three and a half thousand people.

View of the Argus II outdoor unit
Patients who were implanted with a bionic eye, showed the ability not only to distinguish between light and movement, but also to determine objects the size of a cup for tea or even a knife.
The test device was improved — instead of the sixteen photosensitive electrodes, sixty electrodes were mounted into it and called Argus II. In 2007, a multicenter study was initiated in 10 centers in 4 countries in the USA and Europe - a total of 30 patients. In 2012, Argus II received permission for commercial use in Europe, a year later in 2013 - in the United States. In Russia, there is no permission.
To this day, these studies are subsidized by government funds, in the US there are three - the National Eye Institute, the Department of Energy, and the National Science Foundation, as well as a number of research laboratories.
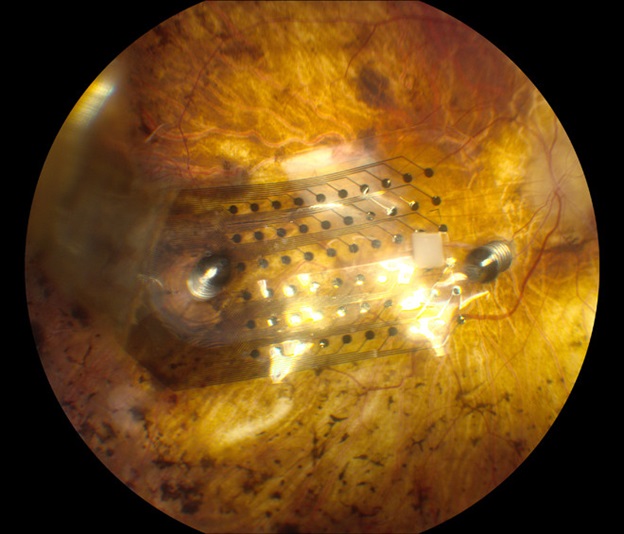
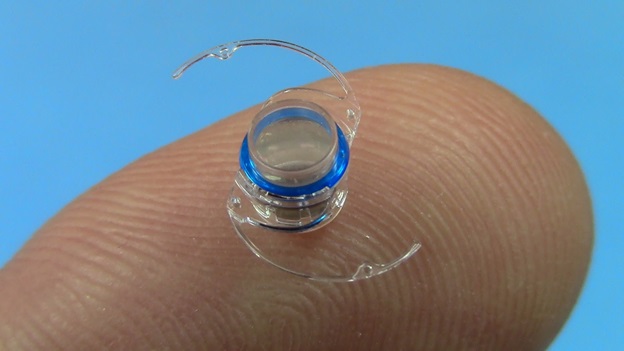
It looks like a chip on the surface of the retina
The prosthesis model was designed by Claude Veraart at the University of Louvain in the form of a spiral cuff of electrodes around the optic nerve at the back of the eye. It connects with a stimulator implanted in a small hole in the skull. The stimulator receives signals from an external camera, which are translated into electrical signals that stimulate the optic nerve directly.
MIVP Scheme
In fact, this device cannot be called a “retinal prosthesis”, since this telescope is implanted in the posterior chamber of the eye and works as a magnifying glass that increases the retinal image by 2.2 or 2.7 times, which makes it possible to reduce the effect on vision by cattle (blind spots) in the central part of the visual field. . Implanted only in one eye, since the presence of the telescope impairs peripheral vision. The second eye works for the periphery. Implanted through a rather large incision of the cornea.
By the way, a similar principle is used in additional Shariott intraocular lenses. I have the most extensive experience of implanting these lenses in Russia and the patients are happy with the results. In this case, cataract phacoemulsification is first performed. Although it is, of course, not 100% bionic eye.
More on this in previous posts:
Telescopic system for the back camera of the eye
In 1995, the development of retinal subretinal prostheses began at the University Eye Clinic Tubingen. A chip with microphotodiodes fit under the retina, which perceived light and transformed it into electrical signals that stimulate ganglion cells like a natural process in photoreceptors of the intact retina.
Of course, photoreceptors are much more sensitive than artificial photodiodes, so they required special amplification.
The first experiments with micro pigs and rabbits were started in 2000, and only in 2009 implants were implanted in 11 patients as part of a clinical pilot study. The first results were encouraging - most patients were able to distinguish day from night, some even could recognize objects - a cup, a spoon, monitor the movement of large objects. By the way, the further fate of these patients was sad - to all participants in the experiment, even those who saw something, according to the signed agreement, the “bionic eyes” were removed and they returned to their original state.
Today Alpha IMS, manufactured by Retina Implant AG Germany, has 1500 electrodes, size 3 × 3 mm, 70 microns thick. After installation under the retina, this allows almost all patients to get some degree of restoration of light perception.
Technically, this complex operation in Germany is performed only in three centers: in Aachen, in Tübingen and Leipzig. In the end, this is done by surgeons from the so-called Cologne school, students of the professor of vitreoretinal surgeon Heinemann, who unfortunately died from leukemia quite early, but all his students became heads of departments in Tubingen, Leipzig and Aachen.
This group of scientists exchanges experience, conducts joint scientific research, these surgeons (in Aachen - Professor Walter (this is his name), in Tübingen - Professor Bartz-Schmitz) have the most extensive experience with bionic eyes, because in this case 7-8 -10 implantations are considered a great experience.
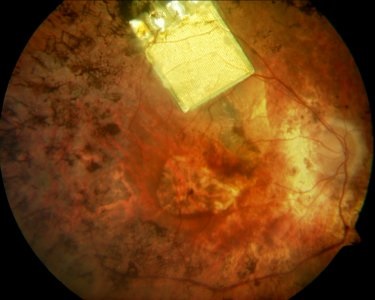
Alpha IMS in the fundus
Joseph Rizzo and John Wyatt from Massachusetts began exploring the possibility of creating a retinal prosthesis in 1989, and conducted stimulation tests on blind volunteers between 1998 and 2000. Today it is the idea of a device of a minimally invasive wireless subretinal neurostimulator consisting of a mass of electrodes, which is placed under the retina in the subretinal space and receives image signals from a camera mounted on a pair of glasses. A chip stimulator decodes image data from a camera and stimulates retinal ganglion cells, respectively. The prosthesis of the second generation collects data and transmits them to the implant through radio-frequency fields from the coil of transmitters mounted on the glasses. The secondary coil of the receiver is sewn around the iris.

MIT Retinal Implant Model
Brothers Alan Chow and Vincent Chow developed a microchip containing 3,500 photodiodes that detect light and convert it into electrical impulses that stimulate healthy retinal ganglion cells. "Artificial silicone retina" does not require the use of external devices. The ASR microchip is a silicon chip with a diameter of 2 mm (the same concept as in computer chips), 25 microns thick, containing ~ 5000 microscopic solar cells called “microphotodiodes”, each of which has its own stimulating electrode.
ASR scheme
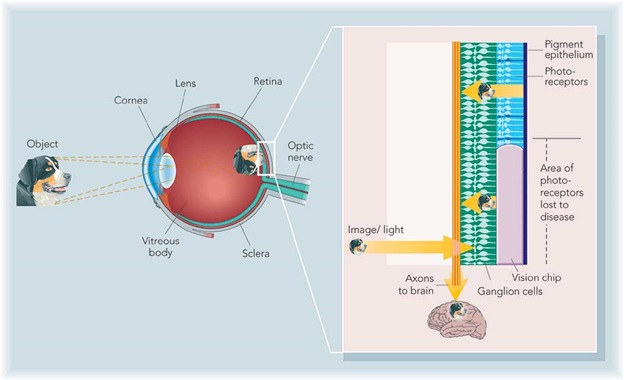
Daniel Palanker and his group at Stanford University have developed a photovoltaic system, which is also the “bionic eye”. The system includes a subretinal photodiode and an infrared projection image system installed on the video glasses.
Information from the video camera is processed in the device and displayed in a pulse infrared (850-915 nm) video image. The infrared image is projected onto the retina through the natural optics of the eye and activates photodiodes in the subretinal implant, which convert light into a pulsed bi-phase electric current at each pixel.
The signal intensity can be further increased by increasing the total voltage provided by the radio frequency drive of the implantable power source.
The similarity between electrodes and neural cells, which is necessary to stimulate high resolution, can be achieved using the effect of retinal migration.
Model Palankera
An Australian team led by Professor Anthony Burkitt is developing two retinal prostheses.
The Wide-View device combines new technologies with materials that have been successfully used for other clinical implants. This approach includes a microchip with 98 stimulating electrodes and is aimed at increasing patient mobility to help them move safely in their environment. This implant will be placed in the suprachoroidal space. The first tests of patients with this device started in 2013.
Bionic Vision Australia is a microchip implant with 1024 electrodes. This implant is placed in the suprachoroidal space. Each prototype consists of a camera attached to a pair of glasses that sends a signal to an implanted microchip, where it is converted into electrical impulses to stimulate the remaining healthy retinal neurons. This information is then transmitted to the optic nerve and visual processing centers of the brain.
The Australian Research Council awarded Bionic Vision Australia a grant of $ 42 million in December 2009, and the consortium was officially launched in March 2010. Bionic Vision Australia brings together a multidisciplinary team, many of whom have extensive experience in developing medical devices, such as the bionic ear.
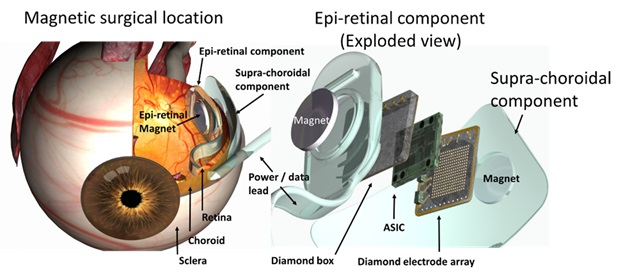
Bionic Vision Australia model
Thanks to researchers from the Institute of Bionics (Melbourne, Australia) and the company evok3d, working on the "bionic eye", people suffering from retinal pigment dystrophy and age-related molecular degeneration will be able to restore vision in the long run. The recovery procedures require the remaining ganglion cells in the patient, a healthy optic nerve and a healthy visual cortex. In this case, the person has the opportunity to regain his sight.
For the manufacture of the prototype of the eye, as well as the mold for its casting, scientists from the Institute of Bionics turned for help to specialists from evok3d, a company specializing in 3D services, and used the ProJet 1200 3D printer to print the “artificial eye”.
It took only four hours to print a prototype on the ProJet 1200, before the advent of 3D printing, it took weeks or even months to make it. This is how 3D printing accelerated the research and production process.
The bionic visual system includes a camera transmitting radio signals to a microchip located at the back of the eye. These signals are converted into electrical impulses that stimulate cells in the retina and optic nerve. Then they are transmitted to the visual areas of the cerebral cortex and are transformed into an image that the patient sees.
Similarly, the function of the Harvard / MIT device (6), except for the stimulatory microcircuit, which is implanted directly into the brain in the primary visual cortex, and not on the retina. First impressions of the implant were good. At the development stage, after Dobel's death, it was decided to transform this project from a commercial one into a project funded by the state.
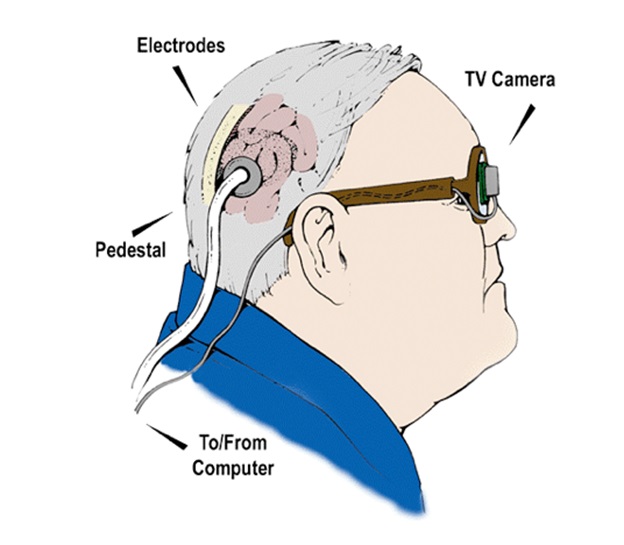
Dobelle Eye Scheme
The laboratory of neural prostheses from the Illinois Institute of Technology in Chicago, is developing a visual prosthesis using intracortical electrodes. In principle, similar to the Dobel system, the use of intracortical electrodes can significantly increase the spatial resolution in the stimulation signals (more electrodes per unit area). In addition, a wireless telemetry system is being developed to eliminate the need for transcranial (intracranial) wires. Electrodes coated with a layer of activated iridium oxide film (AIROF) will be implanted in the visual cortex, located in the occipital lobe of the brain. The outdoor unit will capture the image, process it and generate instructions, which will then be transmitted to the implanted modules via a telemetric link. The circuit decodes instructions and stimulates the electrodes, in turn stimulating the visual cortex. The group develops sensors for external image acquisition and processing systems to accompany specialized implantable modules built into the system. Currently, animal studies and human psychophysical studies are being conducted to test the feasibility of implanting volunteers.

Chip on coin background
Now everything is in the stage, if not primary, but of such secondary development, that there is no question of mass exploitation and the solution of all problems at all. Too few people have been operated on and there is no way to talk about mass production. Currently, this is still a development stage.
The first works began more than 20 years ago. In 2000-2001, something began to turn out in mice. Currently we got the first results in humans. That is such a speed.
While there is something serious, another twenty years may pass. We are at a very, very early stage, at which there is a first positive effect — recognition of contours, light, and not at all — until they can predict to whom it will help, and who cannot.
Surgeons who are engaged in these experiments - count on fingers.
Implanting one prosthesis is for advertising purposes only. These works should be carried out by people who have the opportunity to do 100-200 operations per year in the framework of one project group in order for a critical mass to appear. Then there will be an understanding of when the effect can be expected. Such programs should be subsidized by budget or specialized funds.
Although there is still no perfect model, all existing ones need to be improved, scientists believe that in the future, the electronic eye can replace the function of retinal cells and help people find even the slightest ability to see with diseases such as retinitis pigmentosa, macular degeneration, senile blindness and glaucoma.
If you have your own ideas, how else can technologies be used to return sight to people (even if it is still difficult to implement) - we suggest discussing them below.
And the story of bionic contact lenses, the potential of genome editing, how to hear colors through something implanted in the brain - in the following posts.
So for such cases, the idea of electrical stimulation of the retina or visual cortex was proposed, the creation of a prosthesis that, by the mechanism of action, simulates the actual processes of transmission of electrical signals.
There are several variants of electronic implants; every year new ideas appear, but the term and the Bionic Eye itself were developed by Daniel Palanker, a staff member at Stanford University and his scientific group Biomedical Physics and Ophthalmic Technologies.
The implantation of the Argus II bionic eye model (by the way, the only model that has an EU brand, but not certified in Russia) was performed in Russia in July 2017 for one patient. And from all sources of television broadcasting we heard - now a person will be able to see the world as before. Hundreds of people are asked to put a bionic eye, and some also ask to “implant” the chips for super viewing.
So what do we have today and can a dream come true to see the world after having lost sight?
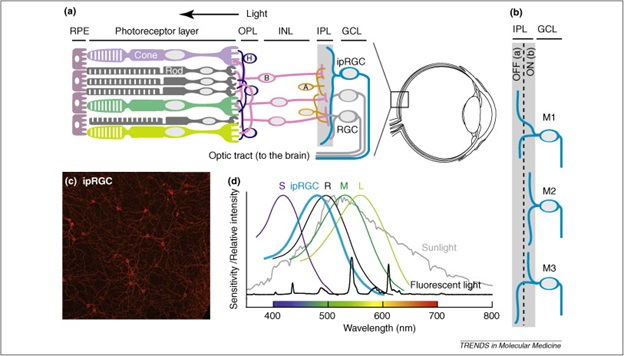
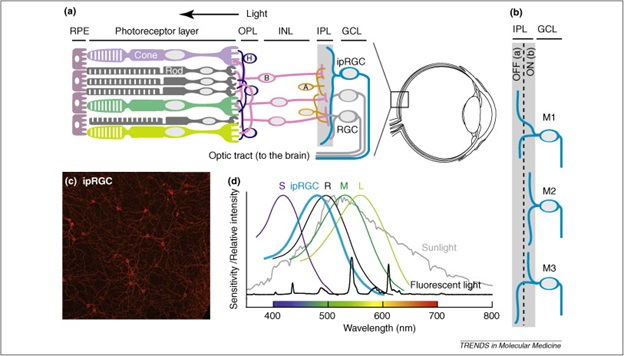
BIOLOGICAL ASPECTS OF THE METHOD
Bionic are called artificial limbs and implantable elements of parts of the human body that are similar in appearance and function to real organs or limbs. Today, bionic arms, legs, hearts, and also organs of hearing successfully help people to have a full life. The purpose of the electronic eye is to help the visually impaired with problems of the retina or optic nerve. Implantable instead of the damaged retina, the device should replace millions of photoreceptor cells of the eye, if not 100%.
Eye technology is similar to that used in hearing aids that help deaf people to hear. Thanks to her, patients are less likely to lose their residual vision, and those who lose their sight see the light and have at least some ability to orient themselves in space.

TECHNOLOGICAL ASPECTS
The general principle of the electronic eye is as follows: a miniature camera is embedded in special glasses, information about the image is transmitted to the device, which converts the image into an electronic signal and sends it to a special transmitter, which in turn sends an electronic signal to an implanted eye or brain the receiver, or information is transmitted through tiny wires to the electrodes attached to the retina, they stimulate the remaining nerves of the retina by sending electrical impulses to the brain cut optic nerves. The device is designed to compensate for lost visual sensations with complete or incomplete loss of vision.
The main conditions for successful operation of the system:
- The presence in the patient's eye and brain of a part of living nerve cells.
- Patients should be people who once were normally seen, since the one who is blind from birth cannot use such devices. Suitable people who have long seen and have a rich visual experience. As a result, they see little, but they have an idea about objects and guess what kind of object it is. In short, the cerebral cortex and the possession of sufficient intelligence must be developed.
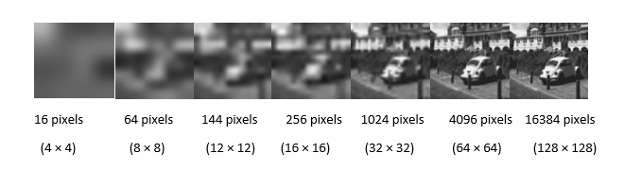
- And, of course, the more pixels there will be in the chip, the clearer the resulting image will be.
- Long service life - as long as the life of these devices, no one knows. The first implantation of bionic eyes in Germany ended with the fact that after a year all patients were removed. Even to those who saw something. This was even written in the German press.
- Technological way to recharge. Now they work on the principle of induction, not on batteries. Charged like an electric toothbrush.
- Along the way, the issue of oxidation, heating, etc. should be addressed. For example, a perforated structure after implantation may allow the retinal nerve cells to automatically flow from the upper and lower surfaces of the photosensor through the cavities and connect, as well as reduce the heating of the pixels and increase their number.
MICROSURGICAL ASPECTS OF PROSTHESIS
These are the most extensive operations. If you describe, for example, the implantation of a subretinal (located under the retina) bionic eye, you need to fully lift the retina, then do an extensive retinectomy (cut off part of the retina), then install this chip under the retina, then retina the retina with a retinal laser, glue the retina with laser coagulation and pour silicone oil . Silicone tamponade is necessary, otherwise PVR (proliferative vitreoretinopathy) will immediately appear and detachment will occur. Yes, there should be no own lens, or it should be replaced with an artificial lens beforehand.
For the operation you need special tools with gentle silicone tips. This is a completely complicated operation, moreover, an orofacial surgeon or an ENT is still needed - they bring the electrodes out through the skin. And it turns out such a device - a chip inside the eye, and in the hands of such a device the size of a mobile phone, with which you can change the signal intensity, it connects to the subcutaneous electrodes. One ophthalmologist-surgeon during the operation is not enough - help from other disciplines is needed, the operation lasts a long 6 hours.
ECONOMIC ASPECTS OF PROSTHESIS
- First, it is expensive. Only the device costs about 150 thousand dollars, that is almost 8.5 million rubles. And all the treatment of one such patient can reach 10 million rubles. This is a model Argus II. Today, in some countries, for example, in Germany, this operation is paid for by insurance.
- Firms engaged in development and production, all over the world live on state subsidies, on grants. This is great - such things should be supported, otherwise there will be no development.
- There is no certificate in Russia for any of the following devices.
MEDICAL ASPECTS OF PROSTHESIS
1. The results are quite modest - after the operation, such people cannot be called sighted, they see a maximum of 0.05, i.e. they can see the contours and determine the direction of movement of the shadow, do not distinguish colors at all, objects can only differ from those that are remembered from the former "sighted" life, for example: "aha - this is probably a banana, because something is semicircular." They see that something is moving on them, they can guess that this is a man, but his face is not distinguished.
2. Under what diseases can a bionic eye be useful?
The first patients are patients with retinitis pigmentosa (retinitis pigmentoza), a disease with a primary disappearance of photoreceptors and secondary atrophy of the optic nerve. In Russia, there are 20-30 thousand such patients, in Germany only a few thousand.
Next in line are patients with geographic atrophic macular degeneration. This is an extremely common age pathology of the eye.
The third will be patients with glaucoma. Glaucoma has not yet been studied, since the atrophy of the optic nerve in this case is primary, so the mode of transmission must be different - bypassing the optic nerve.
Diabetes is the most difficult problem to solve. One of the methods of treating diabetic changes on the retina is laser coagulation over the entire surface. After such a procedure, it is technically impossible to lift the retina due to coagulants - this results in a “sieve”. And if it is not made by a laser, the situation is no better: usually the eye is so damaged that implantation is useless in this case.
3. Unfortunately, the current prototype of the bionic eye does not allow people to see the world around us as we see it. Their goal is to move independently without assistance. Until the mass use of this technology is far, however, scientists will give hope to people who have lost their sight.
CURRENT PROJECTS OF "BIONIC EYES"
In the past few decades, scientists from different countries have been working on the ideas of bionic electronic eyes. Each time, technologies are improving, but no one has yet introduced their product to the market for mass use.
1. Argus retinal prosthesis
The Argus retinal prosthesis is an American project that is fairly well commercialized. The first model was developed by a team of researchers in the early 1990s: Pakistani-born ophthalmologist Mark Hameiun (Mark Humayun, by the way, Professor Sekundo is familiar with him from Johns Hopkins University - at that time he was a resident of the 2nd year, Walter was a student) Eugen Dayan, engineer Howard Phillips, bioengineer Ventay Lew and Robert Greenberg. The first model, released in the late 1990s, by Second Sight had only 16 electrodes.
The “field trials” of the first version of the bionic retina were carried out by Mark Hameiun in six patients with vision loss as a result of retinitis pigmentosa disease in the period from 2002 to 2004. Retinitis pigmentosa is an incurable disease in which a person loses sight. It is observed in approximately one case for every three and a half thousand people.

View of the Argus II outdoor unit
Patients who were implanted with a bionic eye, showed the ability not only to distinguish between light and movement, but also to determine objects the size of a cup for tea or even a knife.
The test device was improved — instead of the sixteen photosensitive electrodes, sixty electrodes were mounted into it and called Argus II. In 2007, a multicenter study was initiated in 10 centers in 4 countries in the USA and Europe - a total of 30 patients. In 2012, Argus II received permission for commercial use in Europe, a year later in 2013 - in the United States. In Russia, there is no permission.
To this day, these studies are subsidized by government funds, in the US there are three - the National Eye Institute, the Department of Energy, and the National Science Foundation, as well as a number of research laboratories.
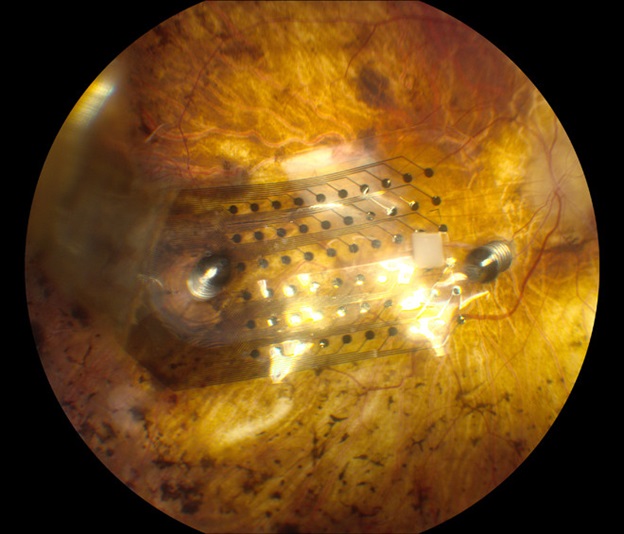
It looks like a chip on the surface of the retina
2. Microsystem-based visual prosthesis (MIVP)
The prosthesis model was designed by Claude Veraart at the University of Louvain in the form of a spiral cuff of electrodes around the optic nerve at the back of the eye. It connects with a stimulator implanted in a small hole in the skull. The stimulator receives signals from an external camera, which are translated into electrical signals that stimulate the optic nerve directly.
MIVP Scheme
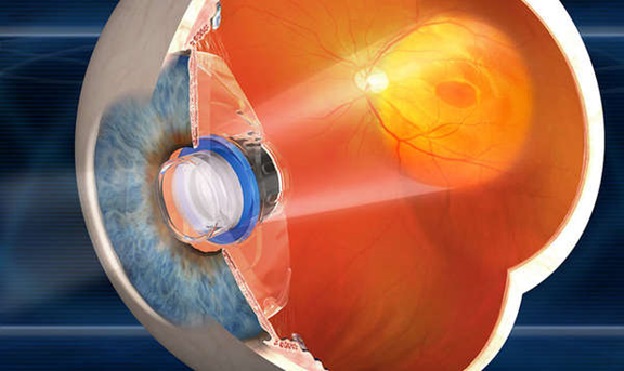
3. Implantable miniature telescope
In fact, this device cannot be called a “retinal prosthesis”, since this telescope is implanted in the posterior chamber of the eye and works as a magnifying glass that increases the retinal image by 2.2 or 2.7 times, which makes it possible to reduce the effect on vision by cattle (blind spots) in the central part of the visual field. . Implanted only in one eye, since the presence of the telescope impairs peripheral vision. The second eye works for the periphery. Implanted through a rather large incision of the cornea.
By the way, a similar principle is used in additional Shariott intraocular lenses. I have the most extensive experience of implanting these lenses in Russia and the patients are happy with the results. In this case, cataract phacoemulsification is first performed. Although it is, of course, not 100% bionic eye.
More on this in previous posts:
- Cataract: it is waiting for you personally (if you live, of course)
- We implant an artificial lens (you will need it after 60 years)
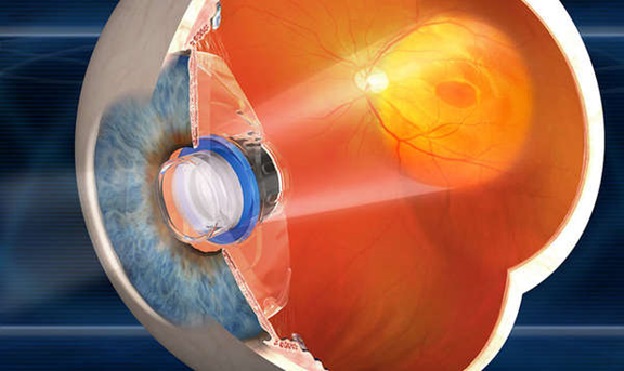
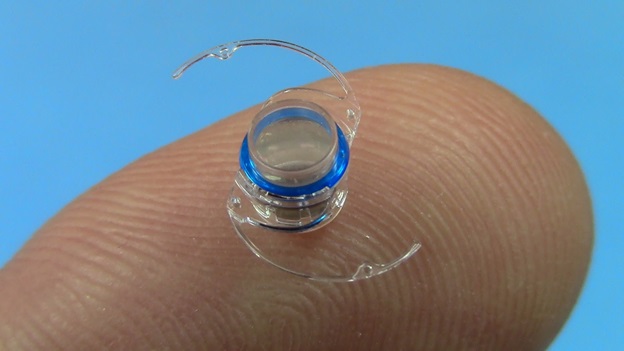
Telescopic system for the back camera of the eye
4. Tübingen MPDA Project Alpha IMS
In 1995, the development of retinal subretinal prostheses began at the University Eye Clinic Tubingen. A chip with microphotodiodes fit under the retina, which perceived light and transformed it into electrical signals that stimulate ganglion cells like a natural process in photoreceptors of the intact retina.
Of course, photoreceptors are much more sensitive than artificial photodiodes, so they required special amplification.
The first experiments with micro pigs and rabbits were started in 2000, and only in 2009 implants were implanted in 11 patients as part of a clinical pilot study. The first results were encouraging - most patients were able to distinguish day from night, some even could recognize objects - a cup, a spoon, monitor the movement of large objects. By the way, the further fate of these patients was sad - to all participants in the experiment, even those who saw something, according to the signed agreement, the “bionic eyes” were removed and they returned to their original state.
Today Alpha IMS, manufactured by Retina Implant AG Germany, has 1500 electrodes, size 3 × 3 mm, 70 microns thick. After installation under the retina, this allows almost all patients to get some degree of restoration of light perception.
Technically, this complex operation in Germany is performed only in three centers: in Aachen, in Tübingen and Leipzig. In the end, this is done by surgeons from the so-called Cologne school, students of the professor of vitreoretinal surgeon Heinemann, who unfortunately died from leukemia quite early, but all his students became heads of departments in Tubingen, Leipzig and Aachen.
This group of scientists exchanges experience, conducts joint scientific research, these surgeons (in Aachen - Professor Walter (this is his name), in Tübingen - Professor Bartz-Schmitz) have the most extensive experience with bionic eyes, because in this case 7-8 -10 implantations are considered a great experience.
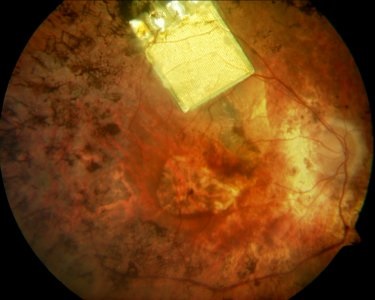
Alpha IMS in the fundus
5. Harvard / MIT Retinal Implant
Joseph Rizzo and John Wyatt from Massachusetts began exploring the possibility of creating a retinal prosthesis in 1989, and conducted stimulation tests on blind volunteers between 1998 and 2000. Today it is the idea of a device of a minimally invasive wireless subretinal neurostimulator consisting of a mass of electrodes, which is placed under the retina in the subretinal space and receives image signals from a camera mounted on a pair of glasses. A chip stimulator decodes image data from a camera and stimulates retinal ganglion cells, respectively. The prosthesis of the second generation collects data and transmits them to the implant through radio-frequency fields from the coil of transmitters mounted on the glasses. The secondary coil of the receiver is sewn around the iris.

MIT Retinal Implant Model
6. Artificial silicon retina (ASR)
Brothers Alan Chow and Vincent Chow developed a microchip containing 3,500 photodiodes that detect light and convert it into electrical impulses that stimulate healthy retinal ganglion cells. "Artificial silicone retina" does not require the use of external devices. The ASR microchip is a silicon chip with a diameter of 2 mm (the same concept as in computer chips), 25 microns thick, containing ~ 5000 microscopic solar cells called “microphotodiodes”, each of which has its own stimulating electrode.
ASR scheme
7. Photovoltaic retinal prosthesis
Daniel Palanker and his group at Stanford University have developed a photovoltaic system, which is also the “bionic eye”. The system includes a subretinal photodiode and an infrared projection image system installed on the video glasses.
Information from the video camera is processed in the device and displayed in a pulse infrared (850-915 nm) video image. The infrared image is projected onto the retina through the natural optics of the eye and activates photodiodes in the subretinal implant, which convert light into a pulsed bi-phase electric current at each pixel.
The signal intensity can be further increased by increasing the total voltage provided by the radio frequency drive of the implantable power source.
The similarity between electrodes and neural cells, which is necessary to stimulate high resolution, can be achieved using the effect of retinal migration.
Model Palankera
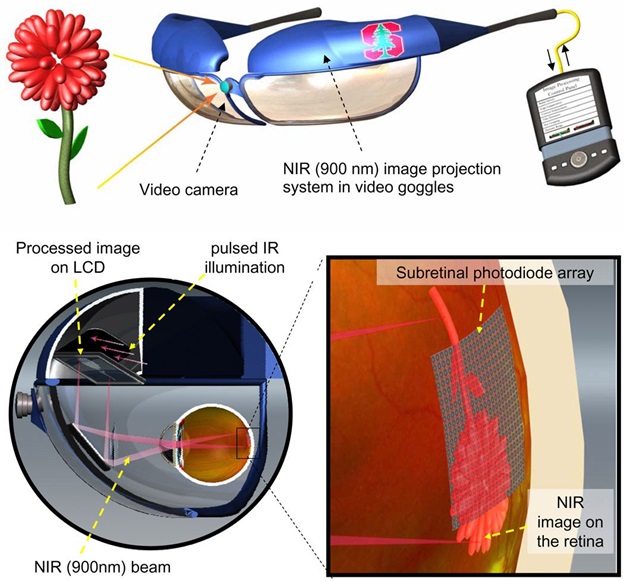
8. Bionic Vision Australia
An Australian team led by Professor Anthony Burkitt is developing two retinal prostheses.
The Wide-View device combines new technologies with materials that have been successfully used for other clinical implants. This approach includes a microchip with 98 stimulating electrodes and is aimed at increasing patient mobility to help them move safely in their environment. This implant will be placed in the suprachoroidal space. The first tests of patients with this device started in 2013.
Bionic Vision Australia is a microchip implant with 1024 electrodes. This implant is placed in the suprachoroidal space. Each prototype consists of a camera attached to a pair of glasses that sends a signal to an implanted microchip, where it is converted into electrical impulses to stimulate the remaining healthy retinal neurons. This information is then transmitted to the optic nerve and visual processing centers of the brain.
The Australian Research Council awarded Bionic Vision Australia a grant of $ 42 million in December 2009, and the consortium was officially launched in March 2010. Bionic Vision Australia brings together a multidisciplinary team, many of whom have extensive experience in developing medical devices, such as the bionic ear.
Bionic Vision Australia model
Thanks to researchers from the Institute of Bionics (Melbourne, Australia) and the company evok3d, working on the "bionic eye", people suffering from retinal pigment dystrophy and age-related molecular degeneration will be able to restore vision in the long run. The recovery procedures require the remaining ganglion cells in the patient, a healthy optic nerve and a healthy visual cortex. In this case, the person has the opportunity to regain his sight.
For the manufacture of the prototype of the eye, as well as the mold for its casting, scientists from the Institute of Bionics turned for help to specialists from evok3d, a company specializing in 3D services, and used the ProJet 1200 3D printer to print the “artificial eye”.
It took only four hours to print a prototype on the ProJet 1200, before the advent of 3D printing, it took weeks or even months to make it. This is how 3D printing accelerated the research and production process.
The bionic visual system includes a camera transmitting radio signals to a microchip located at the back of the eye. These signals are converted into electrical impulses that stimulate cells in the retina and optic nerve. Then they are transmitted to the visual areas of the cerebral cortex and are transformed into an image that the patient sees.
9. Dobelle Eye
Similarly, the function of the Harvard / MIT device (6), except for the stimulatory microcircuit, which is implanted directly into the brain in the primary visual cortex, and not on the retina. First impressions of the implant were good. At the development stage, after Dobel's death, it was decided to transform this project from a commercial one into a project funded by the state.
Dobelle Eye Scheme
10. Intracortical visual prosthesis
The laboratory of neural prostheses from the Illinois Institute of Technology in Chicago, is developing a visual prosthesis using intracortical electrodes. In principle, similar to the Dobel system, the use of intracortical electrodes can significantly increase the spatial resolution in the stimulation signals (more electrodes per unit area). In addition, a wireless telemetry system is being developed to eliminate the need for transcranial (intracranial) wires. Electrodes coated with a layer of activated iridium oxide film (AIROF) will be implanted in the visual cortex, located in the occipital lobe of the brain. The outdoor unit will capture the image, process it and generate instructions, which will then be transmitted to the implanted modules via a telemetric link. The circuit decodes instructions and stimulates the electrodes, in turn stimulating the visual cortex. The group develops sensors for external image acquisition and processing systems to accompany specialized implantable modules built into the system. Currently, animal studies and human psychophysical studies are being conducted to test the feasibility of implanting volunteers.

Chip on coin background
TOTAL
Now everything is in the stage, if not primary, but of such secondary development, that there is no question of mass exploitation and the solution of all problems at all. Too few people have been operated on and there is no way to talk about mass production. Currently, this is still a development stage.
The first works began more than 20 years ago. In 2000-2001, something began to turn out in mice. Currently we got the first results in humans. That is such a speed.
While there is something serious, another twenty years may pass. We are at a very, very early stage, at which there is a first positive effect — recognition of contours, light, and not at all — until they can predict to whom it will help, and who cannot.
Surgeons who are engaged in these experiments - count on fingers.
Implanting one prosthesis is for advertising purposes only. These works should be carried out by people who have the opportunity to do 100-200 operations per year in the framework of one project group in order for a critical mass to appear. Then there will be an understanding of when the effect can be expected. Such programs should be subsidized by budget or specialized funds.
Although there is still no perfect model, all existing ones need to be improved, scientists believe that in the future, the electronic eye can replace the function of retinal cells and help people find even the slightest ability to see with diseases such as retinitis pigmentosa, macular degeneration, senile blindness and glaucoma.
If you have your own ideas, how else can technologies be used to return sight to people (even if it is still difficult to implement) - we suggest discussing them below.
And the story of bionic contact lenses, the potential of genome editing, how to hear colors through something implanted in the brain - in the following posts.
All Articles