How a tear works, and what happens when an eye dries
I have been engaged in eye biopolymers for about 5 years. In the end, I’ll tell you a little about what is so surprising in Russia in this direction.
But let's start with the fact that tear fluid is a very interesting thing. The fact is that it aligns the surface of the eye to get a smooth lens, it works as an “antivirus” at entry into the body through the eye, it supports several more complex reactions, in addition to the immune ones.
It works as a dust barrier, protects the eyes from scratches as a lubricant, kills exogenous bacteria with its immune responses. As the eyelids move, the fluid is smeared over the surface of the cornea and forms a pericorneal film that aligns the front lens of the eye. This is important because irregularities from 0.3 µm² in size are already well visible and distort vision. In addition, humidity is important for the layer of non-keratinous epithelium of the eye - thanks to this layer, our eyes can eventually get enough oxygen.
Contrary to popular belief, the lacrimal gland does quite a bit to permanently protect the eye. This is a kind of backup storage for the fluid needed to wash the eye, or to enhance the immunity of the eye (for example, as a result of emotional distress). The main lacrimal fluid, which makes the eye constantly wet, comes from the relatively small glands of Krause and Wolfring.
A tear is made from the secretions of the glands and cells from the mucous membrane of the eye, some components also come from the vessels of the eye. The three main components of tears are lipids, mucins and water.
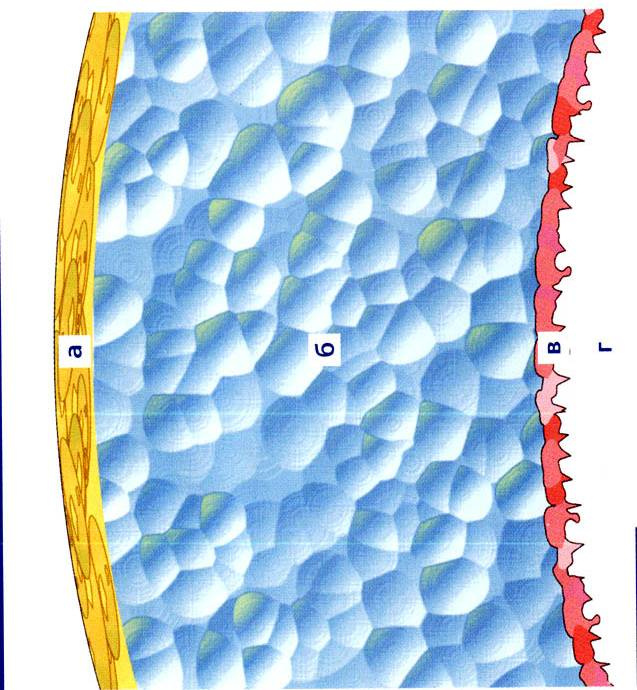
The yellow layer A is lipids, the blue layer B is a watery liquid, the red layer B is the mucin layer, the cornea G is already on. Thickness is from 6 to 10 microns.
The upper lipid layer is produced by the meibomian glands (in the eyelids), the Zeiss sebaceous glands in the hair sacs at the roots of the eyelashes, the Mole glands (located nearby, these are slightly modified small sweat glands). Threefold duplication of the system is necessary because of the very great importance of the eyes for the organism, and, accordingly, the very great importance of this layer of tears for the work of the eye.
This lipid film does not allow the tear to evaporate quickly, seals the eye when it closes (so that the nasty bacteria do not crawl inside while you sleep), reduces the tension of the liquid and smoothes the surface of the lens, plus does not allow external sweat from the skin to damage the eye. Sometimes it happens that a patient complains of dry eyes or immediately receives an objective diagnosis of dry eye syndrome during normal or elevated tear production - this is just the case of damage to lipid products for this film during normal operation of the remaining glands of tear products. Most often, this layer is damaged as a result of blepharitis, in which the ducts of meibomian glands in the thickness of the eyelids are blocked.
CVD is, in fact, a violation of tear production. There are several reasons for its occurrence:
Systemic - congenital, hereditary, as a result of hormonal diseases, menopause, diabetes, less often - with systemic infections. In this situation, the very properties of eye tissue change, which leads to its dystrophy. The prevalence is 1%, and if you don’t have one among your relatives, you probably don’t need to worry. With acquired dry eye syndrome, the circumstances are such that, most likely, it will worry you least of all in comparison with lesions of other organs.
The most common form is blepharoconjunctival. These are diseases of the eyelids and the mucous membrane of the eye. Inflammation unbalances the composition of the tears, and then the eye loses its protection and everything becomes much more fun. For the doctor, not for the patient. Causes: infections, incomplete closure of the eyelids, allergies and other similar factors. The prevalence of 58%.
Another 34% percent - exogenous form (also accompanied by blepharitis). Causes: EMI-impulses (communicators suffer), overdried air, smoke, smog, cigarette smoke - a tear begins to evaporate faster. If you reduce the blink of the eye, then the tear also begins to evaporate quickly. When we talk about dry eye syndrome at work or as a result of working at a computer, this is most often it. More exogenous form cause drugs like hormonal contraceptives, neuroleptics, botulinum toxin injections, wearing contact lenses, ionizing radiation, vitamin deficiency A.
The remaining cases are the corneal form caused by too uneven corneas. For example, after trauma, surgery (especially laser correction, keratectomy, cataract phacoemulsification), dystrophic processes or severe toxicological lesions.
There are also combined forms when there is no obvious “trigger”, but there are a lot of different reasons that have accumulated as it should.
The simplest method for diagnosing the correctness of tear fluid operation is the Schirmer test. Special thorns are inserted into your eyes on pieces of paper, and then they wait until you start crying. A certain time is cut off, then it is checked how far the pieces of paper are soaked. You need to dial 15 millimeters in 5 minutes. For its implementation, these are the very thorns and pieces of paper, usually every ophthalmologist has them.
The caveat is that patients can cry not only from eye irritation, but also from pain. Then the tears will be more. Therefore, more advanced ophthalmologists use the Jones test. All the same, but first you are waiting for anesthesia.
The method, available only in large diagnostic centers and laboratories - test according to Norn. It shows the tearing time of the tear film. The tear is stained with special solutions, after which you are not blinking in the microscope until the first break appears (visible as an unpainted area). Norm - 10 seconds. Schirmer and Jones tests measure the water component, the Norn sample is a lipid and mucin test.
There are more complex laboratory methods, but they are not as fast. If they are appointed to you, this usually means your forced deep immersion into the topic, so for now let's skip. If you are not lucky - you will understand the situation.
The problem is very frequent. A different treatment is prescribed, which reduces to eliminating the cause of the occurrence of the disorder (this may be a rare surgery if there was an injury; hormonal effects, etc.), but almost always we are talking about two basic things:
Unfortunately, the latter is usually forgotten, or is simply not prescribed, since blepharitis may not be at the beginning. But he is very likely to occur later.
But let's start with tears. Of course, a couple of centuries ago, salt solutions worked perfectly, then approximately in the 80s natural polymers became widespread - solutions on the serum of dry plasma or patient’s blood. Since not every patient was eager to become an honorary donor (even for himself), the synthesis of artificial polymers was needed. They were introduced into the eye very often, which caused a lot of inconvenience to patients. Then there were long-acting drugs:

The choice depends on the specific condition of the patient. Sometimes they prescribe two drugs for joint action.
Also during treatment, hydrogel protective lenses are used, which must be worn continuously and in parallel with the administration of drugs. It is assumed that they protect the eyes long enough for the drugs to begin to act normally.
It is also possible to increase tear production by affecting the glands or reducing the viscosity of the tear due to the impact on the mucin layer (it is limited - if there are problems with mucin, it is not applicable, plus there are rather unpleasant side effects, but sometimes the method turns out to be suitable).
Then, in fact, surgery. For this purpose, a coating of canned amniotic membrane (only for patients with the corneal form of the syndrome) or autoconjunctiva (according to Kunt) is used or a cornea transplant is performed. It is better not to bring up this story - extremely high risks and almost cosmic price of operations. If you bring - try to go to Germany for the operation. You can also put the collagen plugs for 5-7 days, preventing the flow of tears from the eyes into the nasal cavity. They gradually dissolve, but give a week so that the eye works normally.
The first part of the treatment is protective. In addition, it is often used etiotropic treatment, that is, helping to remove the causes of the disease. These are reducing agents, antibiotics, desensitization, efferent therapy and reparative therapy.
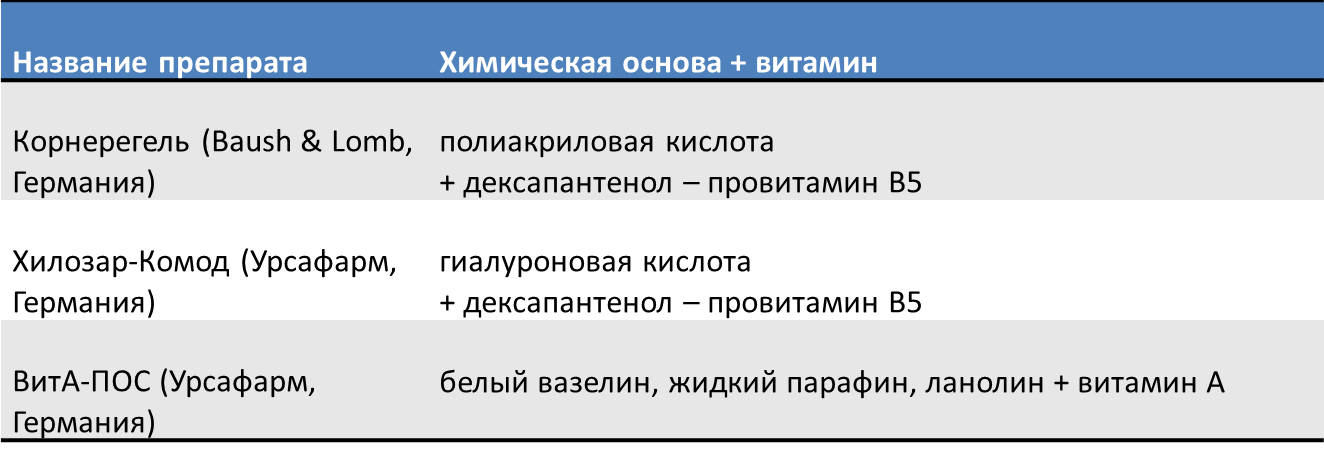
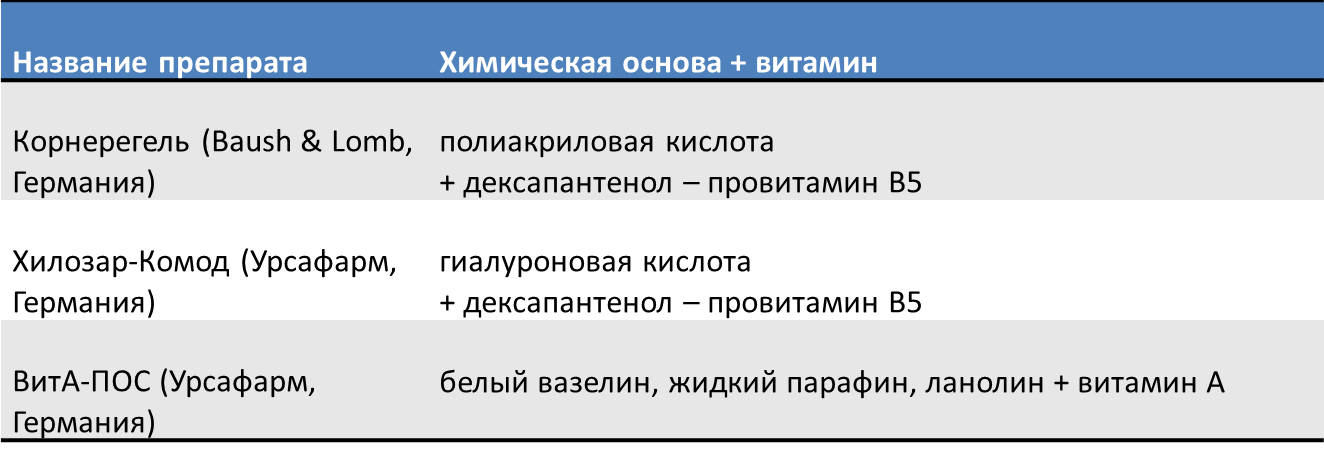
Reparative therapy - restoring the integrity of the cornea, mucous membrane, improving metabolism. Here are the main drugs:
You can apply and autoservice blood (drug from the patient's blood).
When blepharoconjunctival SSG form and in situations where blepharitis is more than possible as the disease progresses (that is, in most cases), warm compresses, eyelid massage and hygiene products are prescribed. It was here that our laboratory became one of the unique world phenomena. We developed the Blefarogel and Blefarogel-2 gels (yes, in the 90s we were more engaged in science than marketing). Blefarogel is applied on the eyelids and acts as follows: based on hyaluronic acid, which slowly clears the excretory ducts of the sebaceous, meibomian, sweat glands of the eyelids from traffic jams. Here, by the way, confusion arises - for some reason, the ladies in the cosmetology forums, seeing a familiar biopolymer, decide that it removes wrinkles. No, blefarogel - it is for another. But yes, the hydrobalance of the eyelid skin is still normal, its elasticity increases. Further, the aloe extract is activated - it is antiseptic and helps the trophic. As a result, swelling, hyperemia is removed. And Blefarogel 2 is more serious. Sulfur preparations that aptly kill parasites, in particular, Demodex ticks, are also included there - a lot of blepharitis is associated with them.
As a result, in parallel with the appointment of massage or phonophoresis (magnetophoresis, electrophoresis), the CVL is successfully cured, since the exchange of fluids and the functioning of the glands are normalized. Treated the cause of the disease. In addition, both tools can be used for the prevention of CVG, as well as simply to improve trophism, especially if the person is not in comfortable working conditions.
Historically, at the end of the 1990s, my company worked on biopolymers for cosmetics at the institute laboratory. Doctors came to us who needed our developments - they used our hyaluronic acid gels for treatment during a series of tests, and the first tests showed the result. Medical developers showed us what we need to come to, and polymer developers developed the necessary tools. Prior to the start of our work, for example, on Blefarogel, 2 patients with demodicosis were transferred from optics to KVD and back. 3-4 years we tested the first tools and certified them as hygienic. Then a series of studies was needed and already documents for a medical product. Initially, we were very lucky that from the very first experiments we worked exclusively with pure hyaluronic acid (about the importance of this and methods of synthesis a little later).
A little later, I will tell you more directly about the process of developing biopolymer agents, if interested. In the meantime, here you can look at our production of gels for ultrasound and cosmetic preparations , based on all the same polymer development. Well, here's more details about the SSG .
But let's start with the fact that tear fluid is a very interesting thing. The fact is that it aligns the surface of the eye to get a smooth lens, it works as an “antivirus” at entry into the body through the eye, it supports several more complex reactions, in addition to the immune ones.
It works as a dust barrier, protects the eyes from scratches as a lubricant, kills exogenous bacteria with its immune responses. As the eyelids move, the fluid is smeared over the surface of the cornea and forms a pericorneal film that aligns the front lens of the eye. This is important because irregularities from 0.3 µm² in size are already well visible and distort vision. In addition, humidity is important for the layer of non-keratinous epithelium of the eye - thanks to this layer, our eyes can eventually get enough oxygen.
Contrary to popular belief, the lacrimal gland does quite a bit to permanently protect the eye. This is a kind of backup storage for the fluid needed to wash the eye, or to enhance the immunity of the eye (for example, as a result of emotional distress). The main lacrimal fluid, which makes the eye constantly wet, comes from the relatively small glands of Krause and Wolfring.
A tear
A tear is made from the secretions of the glands and cells from the mucous membrane of the eye, some components also come from the vessels of the eye. The three main components of tears are lipids, mucins and water.
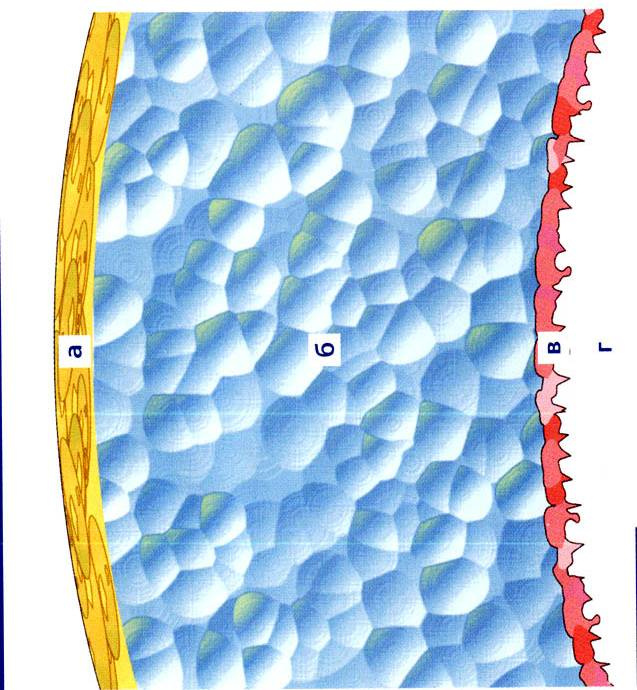
The yellow layer A is lipids, the blue layer B is a watery liquid, the red layer B is the mucin layer, the cornea G is already on. Thickness is from 6 to 10 microns.
The upper lipid layer is produced by the meibomian glands (in the eyelids), the Zeiss sebaceous glands in the hair sacs at the roots of the eyelashes, the Mole glands (located nearby, these are slightly modified small sweat glands). Threefold duplication of the system is necessary because of the very great importance of the eyes for the organism, and, accordingly, the very great importance of this layer of tears for the work of the eye.
This lipid film does not allow the tear to evaporate quickly, seals the eye when it closes (so that the nasty bacteria do not crawl inside while you sleep), reduces the tension of the liquid and smoothes the surface of the lens, plus does not allow external sweat from the skin to damage the eye. Sometimes it happens that a patient complains of dry eyes or immediately receives an objective diagnosis of dry eye syndrome during normal or elevated tear production - this is just the case of damage to lipid products for this film during normal operation of the remaining glands of tear products. Most often, this layer is damaged as a result of blepharitis, in which the ducts of meibomian glands in the thickness of the eyelids are blocked.
What causes dry eye syndrome?
CVD is, in fact, a violation of tear production. There are several reasons for its occurrence:
Systemic - congenital, hereditary, as a result of hormonal diseases, menopause, diabetes, less often - with systemic infections. In this situation, the very properties of eye tissue change, which leads to its dystrophy. The prevalence is 1%, and if you don’t have one among your relatives, you probably don’t need to worry. With acquired dry eye syndrome, the circumstances are such that, most likely, it will worry you least of all in comparison with lesions of other organs.
The most common form is blepharoconjunctival. These are diseases of the eyelids and the mucous membrane of the eye. Inflammation unbalances the composition of the tears, and then the eye loses its protection and everything becomes much more fun. For the doctor, not for the patient. Causes: infections, incomplete closure of the eyelids, allergies and other similar factors. The prevalence of 58%.
Another 34% percent - exogenous form (also accompanied by blepharitis). Causes: EMI-impulses (communicators suffer), overdried air, smoke, smog, cigarette smoke - a tear begins to evaporate faster. If you reduce the blink of the eye, then the tear also begins to evaporate quickly. When we talk about dry eye syndrome at work or as a result of working at a computer, this is most often it. More exogenous form cause drugs like hormonal contraceptives, neuroleptics, botulinum toxin injections, wearing contact lenses, ionizing radiation, vitamin deficiency A.
The remaining cases are the corneal form caused by too uneven corneas. For example, after trauma, surgery (especially laser correction, keratectomy, cataract phacoemulsification), dystrophic processes or severe toxicological lesions.
There are also combined forms when there is no obvious “trigger”, but there are a lot of different reasons that have accumulated as it should.
Diagnostics
The simplest method for diagnosing the correctness of tear fluid operation is the Schirmer test. Special thorns are inserted into your eyes on pieces of paper, and then they wait until you start crying. A certain time is cut off, then it is checked how far the pieces of paper are soaked. You need to dial 15 millimeters in 5 minutes. For its implementation, these are the very thorns and pieces of paper, usually every ophthalmologist has them.
The caveat is that patients can cry not only from eye irritation, but also from pain. Then the tears will be more. Therefore, more advanced ophthalmologists use the Jones test. All the same, but first you are waiting for anesthesia.
The method, available only in large diagnostic centers and laboratories - test according to Norn. It shows the tearing time of the tear film. The tear is stained with special solutions, after which you are not blinking in the microscope until the first break appears (visible as an unpainted area). Norm - 10 seconds. Schirmer and Jones tests measure the water component, the Norn sample is a lipid and mucin test.
There are more complex laboratory methods, but they are not as fast. If they are appointed to you, this usually means your forced deep immersion into the topic, so for now let's skip. If you are not lucky - you will understand the situation.
What if a tear is generated incorrectly?
The problem is very frequent. A different treatment is prescribed, which reduces to eliminating the cause of the occurrence of the disorder (this may be a rare surgery if there was an injury; hormonal effects, etc.), but almost always we are talking about two basic things:
- Appointment of tear replacement therapy (so that the eye does not suffer further as the loss of protection due to the disease).
- Improve trophism, prevention or treatment of associated inflammatory processes.
Unfortunately, the latter is usually forgotten, or is simply not prescribed, since blepharitis may not be at the beginning. But he is very likely to occur later.
But let's start with tears. Of course, a couple of centuries ago, salt solutions worked perfectly, then approximately in the 80s natural polymers became widespread - solutions on the serum of dry plasma or patient’s blood. Since not every patient was eager to become an honorary donor (even for himself), the synthesis of artificial polymers was needed. They were introduced into the eye very often, which caused a lot of inconvenience to patients. Then there were long-acting drugs:

The choice depends on the specific condition of the patient. Sometimes they prescribe two drugs for joint action.
Also during treatment, hydrogel protective lenses are used, which must be worn continuously and in parallel with the administration of drugs. It is assumed that they protect the eyes long enough for the drugs to begin to act normally.
It is also possible to increase tear production by affecting the glands or reducing the viscosity of the tear due to the impact on the mucin layer (it is limited - if there are problems with mucin, it is not applicable, plus there are rather unpleasant side effects, but sometimes the method turns out to be suitable).
Then, in fact, surgery. For this purpose, a coating of canned amniotic membrane (only for patients with the corneal form of the syndrome) or autoconjunctiva (according to Kunt) is used or a cornea transplant is performed. It is better not to bring up this story - extremely high risks and almost cosmic price of operations. If you bring - try to go to Germany for the operation. You can also put the collagen plugs for 5-7 days, preventing the flow of tears from the eyes into the nasal cavity. They gradually dissolve, but give a week so that the eye works normally.
The first part of the treatment is protective. In addition, it is often used etiotropic treatment, that is, helping to remove the causes of the disease. These are reducing agents, antibiotics, desensitization, efferent therapy and reparative therapy.
Reparative therapy - restoring the integrity of the cornea, mucous membrane, improving metabolism. Here are the main drugs:
You can apply and autoservice blood (drug from the patient's blood).
When blepharoconjunctival SSG form and in situations where blepharitis is more than possible as the disease progresses (that is, in most cases), warm compresses, eyelid massage and hygiene products are prescribed. It was here that our laboratory became one of the unique world phenomena. We developed the Blefarogel and Blefarogel-2 gels (yes, in the 90s we were more engaged in science than marketing). Blefarogel is applied on the eyelids and acts as follows: based on hyaluronic acid, which slowly clears the excretory ducts of the sebaceous, meibomian, sweat glands of the eyelids from traffic jams. Here, by the way, confusion arises - for some reason, the ladies in the cosmetology forums, seeing a familiar biopolymer, decide that it removes wrinkles. No, blefarogel - it is for another. But yes, the hydrobalance of the eyelid skin is still normal, its elasticity increases. Further, the aloe extract is activated - it is antiseptic and helps the trophic. As a result, swelling, hyperemia is removed. And Blefarogel 2 is more serious. Sulfur preparations that aptly kill parasites, in particular, Demodex ticks, are also included there - a lot of blepharitis is associated with them.
As a result, in parallel with the appointment of massage or phonophoresis (magnetophoresis, electrophoresis), the CVL is successfully cured, since the exchange of fluids and the functioning of the glands are normalized. Treated the cause of the disease. In addition, both tools can be used for the prevention of CVG, as well as simply to improve trophism, especially if the person is not in comfortable working conditions.
Historically, at the end of the 1990s, my company worked on biopolymers for cosmetics at the institute laboratory. Doctors came to us who needed our developments - they used our hyaluronic acid gels for treatment during a series of tests, and the first tests showed the result. Medical developers showed us what we need to come to, and polymer developers developed the necessary tools. Prior to the start of our work, for example, on Blefarogel, 2 patients with demodicosis were transferred from optics to KVD and back. 3-4 years we tested the first tools and certified them as hygienic. Then a series of studies was needed and already documents for a medical product. Initially, we were very lucky that from the very first experiments we worked exclusively with pure hyaluronic acid (about the importance of this and methods of synthesis a little later).
A little later, I will tell you more directly about the process of developing biopolymer agents, if interested. In the meantime, here you can look at our production of gels for ultrasound and cosmetic preparations , based on all the same polymer development. Well, here's more details about the SSG .
All Articles