German doctors have grown transgenic skin for 80% of the child’s body

Left: Demonstration of normal functionality and elasticity of transgenic skin. Right: lack of blistering in places where biopsy was taken after transplantation
In June 2015, a seven-year-old boy entered the burn ward of the German hospital, whose entire skin was covered with blisters. Their cause was not burns, but a rare genetic disease called epidermolysis bullosa (epidermolysis bullosa). Because of him, the child lost 80% of the outer layer of the epidermis, opening the way to life-threatening infections.
The cause of this genetic disease is a mutation in the genes encoding laminin-332, a key component of the basement membranes, a thin cell-free layer that separates the connective tissue from the epithelium. Patients with such a diagnosis often die at an early age, and the survivors develop chronic damage to the skin and mucous membranes, which makes life difficult (such children cannot literally touch) and leads to skin cancer.
Given the threat to the life of the child, he was considered a suitable patient for testing the regeneration of almost complete epidermis from transgenic stem cells. An international group of European scientists and physicians have grown and transplanted a new skin to the boy , which covers 80% of the body, including almost entirely his arms, legs and back.
Scientists have experimented with this method of gene therapy before, growing small fragments of skin from the patient's stem cells. For example, a group from Stanford University (USA) is working on the same project together with the biotechnology company Abeona, but they say that they have never thought about a complete transplant of the patient's skin, and grow only small sheets for damaged areas. This operation in Germany is the world's largest demonstration of transgenic skin.

Patient with a loss of 80% of the outer layer of the epidermis. Photo: Nature magazine
There are three main types of epidermolysis bullosa. In this case, the boy's cells contained mutated copies of the LAMB3 gene, which, as already mentioned, encodes laminin-332 and helps strengthen the epidermis.
Researchers removed cells from intact skin. Stem cells isolated from these samples were able to recreate new skin (as is well known, the process of regeneration of the epidermis is constantly taking place in humans). As part of the transgenic operation, stem cells infected a specially designed virus that is programmed to change mutated copies of the LAMB3 gene to normal copies. After a kind of “genetic transcoding,” scientists began to grow sheets of healthy stem cells on a plastic base, which were then implanted onto the patient's skin.
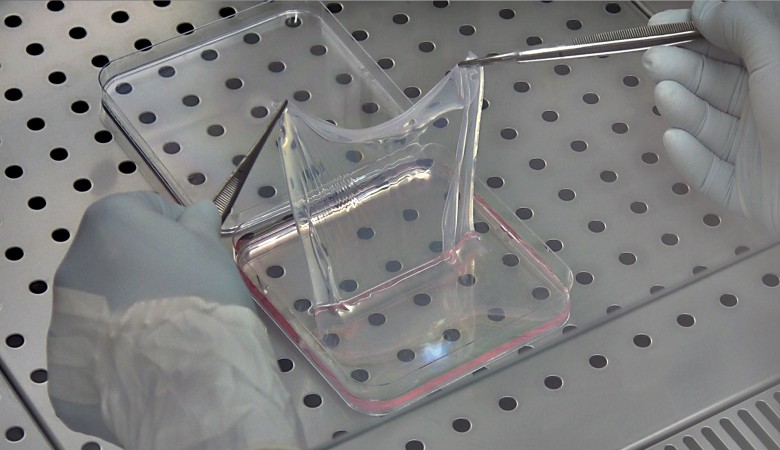
Leaf of transgenic stem cells. Photo: Center for Regenerative Medicine, University of Modena and Reggio Nel Emilia (Italy)
The grown sheets had a different size: from 5 × 7 cm to 13 × 13 cm.
Skin transplantation on 80% of the body surface required three operations. Since then, more than 21 months have passed. Skin regeneration in reconstructed areas is normal, without blistering. The child was finally able to return to school, and even plays football, scientists say. They believe that it will no longer be necessary to carry out repeated operations in order to implant new sheets of stem cells. Apparently, the genetic disease is completely cured - most of the incorrect copies of the gene are replaced with the correct version. The new skin will remain with the person forever and will constantly regenerate with the already correct LAMB3 gene.

Skin regeneration with transgenic crops. The implantation of plastic sheets with genetically modified stem cells on the left arm and back is shown, the healing process after one month (f, h) and after four months (i). Photo: Nature
According to experts, gene therapy is the best treatment option for patients with epidermolysis bullosa, because there is no medicine for this disease. Worldwide, this type of genetic mutation affects about 500,000 people. For them, the ability to get real healthy transgenic skin means the beginning of a new, full life.
The scientific article “Regeneration of the complete human epidermis using transgenic stem cells” was published on November 8, 2017 in the journal Nature (doi: 10.1038 / nature24487, pdf ).
All Articles