In the process of ontogenesis, various morphological disorders occur in the reproductive system of the girl. One of them is the septum in the uterus. This is a very serious pathology, which can lead to infertility or miscarriage of the child.
Medical certificate
Laparoscopy and hysteroscopy are diagnostic methods prescribed when there is a strong indication. At the child planning stage, they are not required. Obtaining good results of ultrasound and gynecological examinations annually, a woman may not even be aware of future problems with bearing the fetus. Spontaneous miscarriages are able to repeat many times until an advanced diagnosis using invasive techniques is completed.
One of the most common problems characteristic of the clinical picture described above is an incomplete septum in the uterus. This is a congenital pathology, found in 2-3% of cases. It is defined as the division of the genital organ into 2 parts of different lengths. Sometimes the septum reaches the cervical canal. In this case, it is called complete. It is possible to get pregnant and subsequently successfully bear a child only after the appropriate operation.
Pathogenesis of pathology
Approximately 3-4 gestational weeks in the fetus, and regardless of its gender, the primary sex gland is formed. In a boy at 7 weeks, she transforms into 2 testicles and begins to produce testosterone. In girls, the ovaries form a little later - about 8-10 weeks.
By the fifth gestational week, the embryo has 2 pairs of reproductive ducts: Wolf and Müller. If by week 8 they do not begin to experience the effects of testosterone, the Wolf ducts partially die. Their residual site takes part in the development of the kidney.
Muller ducts gradually come together and grow together, forming a uterine cavity. The common wall, with which they grow together, dissolves by the 20th gestational week. This is necessary for the formation of a single cavity. If this does not happen, an anomaly of development appears - an intrauterine septum.

Main reasons
The development of the anomaly is not associated with genetic features. Doctors associate its occurrence with the impact on the body of a pregnant woman of external factors. The period from 10 to 20 weeks is especially dangerous.
Adverse agents may include:
- harmful habits of the future mother in childbirth;
- severe toxicosis during pregnancy;
- mother-transmitted infections related to the TORCH group (rubella, toxoplasmosis, herpes, etc.);
- diabetes, as already available before conception, and acquired;
- taking toxic medications;
- violations in the formation and attachment of the placenta;
- poor mother nutrition;
- exposure to ionizing radiation.
Most often, the septum in the uterus does not manifest itself for a long time. That is why the representatives of the fair sex learn about the pathology by chance, for example, during a diagnostic examination.

Clinical picture
Pathology has nonspecific symptoms, which in each case appear individually. First of all, the appearance of very painful periods in young girls. However, this is not a reason to see a doctor, because they do not know how normal menstruation goes.
The second obvious symptom is heavy uterine bleeding. Usually they occur in the middle of the cycle and resemble very painful periods. The third and most rare manifestation of the disease is primary amenorrhea. This is a condition when menstruation does not occur at all.
Pathology, as a rule, is detected only during an in-depth examination on the impossibility of conception or habitual miscarriage. An abnormal structure of the kidneys detected by ultrasound is also considered a cause for concern. In this case, the doctor recommends a thorough check of the functioning of the organs of the reproductive system.

Varieties of anomalies
As already noted a little higher, depending on the degree of separation of the genital organ, two pathologies are distinguished:
- Complete partition. It stretches from the bottom of the uterus and reaches the cervix. In some cases, goes to the vagina. It is not possible to take out a child.
- Incomplete partition. It partially covers the volume of the uterus. This is the most favorable variant of the course of the disease, but also does not exclude problems with conception.
The partition is of various thicknesses. It can be located both longitudinally and transversely.
In some cases, the anomaly is combined with other pathologies of the reproductive system. We are talking about a bicorn and saddle uterus. They do not interfere with natural conception, but pregnancy can occur with complications.
Diagnostic Methods
The septum in the uterus is very difficult to diagnose. A standard examination on a gynecological chair does not allow it to be detected. Ultrasound of the pelvic organs with this problem also turns out to be uninformative. Hysterosalpingography, which implies an x-ray of the uterine cavity and fallopian tubes, is useful only in 50% of cases. Even CT and MRI with this anomaly almost completely lose their diagnostic value.
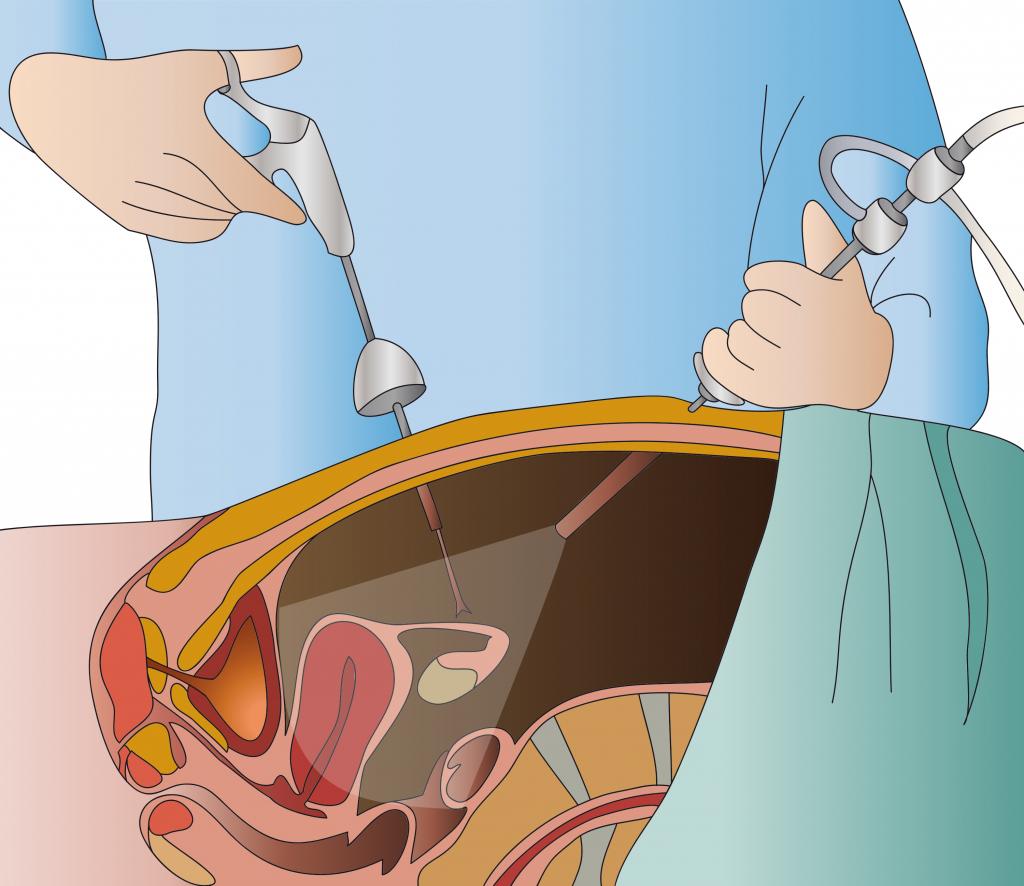
The gold standard in the detection of pathology is the combination of hysteroscopy and laparoscopy. In the first case, an optical device is inserted into the uterine cavity, and then it is filled with gas or liquid. The procedure is performed under general anesthesia. The study allows you to examine the membrane of connective tissue, evaluate its length and thickness, and also evaluate the shape of the uterus. It is recommended to carry it out in the first half of the cycle.
With laparoscopy, manipulation tools are inserted through small punctures on the abdomen. The procedure helps to evaluate the condition of the genital organ and its symmetry, the functionality of the fallopian tubes and ovaries.
Based on the results of the examination, the doctor prescribes therapy.
Treatment features
Removal of the septum in the uterus is carried out surgically using therapeutic hysteroscopy under the control of a laparoscope. The main indications for the procedure are infertility and several history of miscarriages. However, some doctors are against such an operation. Independent conception and successful bearing is possible in 50% of cases.
Hysteroscopy begins with an extension of the organ cavity using an isotonic solution. Then the doctor proceeds to a phased excision of the septum through the cervical canal. The main tool is special scissors. Their use avoids internal bleeding.
In the case of a thick-walled septum in the uterus, hysteroresectoscopy is considered the optimal method for its removal. It is largely similar to standard hysteroscopy. However, the electrodes in the form of a knife or a loop act as tools for manipulation. During the procedure, tissue coagulation is also performed. Its main advantage is the low invasiveness of the inner layer of the uterus. Complete restoration of the mucous layer is observed 3 months after the intervention.
The use of hysteroscopy and laparoscopy is justified. Laparoscopic control helps:
- Assess the size and shape of the uterus, identify the nature of the anomaly.
- Determine the progress of the procedure. A special lighting system transmits the organ through the muscle layer. This approach avoids perforation.
- If necessary, move the bowel loops to the side so as not to damage them during surgery.
- In case of damage to the genital organ, the perforated hole can be sutured quickly.
The choice of a specific method of intervention remains with the doctor. Moreover, he must take into account the presence of concomitant health problems in women.
Postoperative period
After surgery, all patients are prescribed hormone therapy. It is a kind of prevention of synechiae and helps to accelerate the epithelization of the wound surface. The course of treatment is 2-3 months. Also, antibiotics are prescribed to prevent the occurrence of inflammatory processes.

Possible complications
The operation is sometimes accompanied by a breakthrough of the genital organ wall. In addition, resection contributes to the thinning of the uterine fundus. This violation can cause organ rupture during pregnancy. Therefore, the entire gestation period should be under the supervision of a good gynecologist.
Pregnancy planning is allowed no earlier than 13 months after surgery. Throughout the period, a woman is recommended to use barrier contraceptives.
Pathology and pregnancy
The presence of a partition affects a woman's ability to have children.
First of all, it can be the main cause of infertility. In 21-28% of women with this defect, primary infertility is diagnosed. This means that pregnancy has never occurred. In 12-19% of cases, this condition is secondary. The woman has already managed to give birth to one child, but after all attempts at conception fail.
On the other hand, during pregnancy with a septum of the uterus there is a risk of miscarriage. The likelihood persists even in the second trimester and provided that the fetus is attached to the organ wall. One of the reasons for the interruption is the non-closure of the walls of the cervical canal. As a result, the cervix loses its ability to resist intrauterine pressure, which only increases as the fetus grows and develops. Without timely medical correction, a miscarriage may occur. In addition, the septum inside the genital organ does not allow the cavity to grow in proportion to the growing child.
However, medical statistics are very comforting. In 50% of cases, women with a similar anomaly manage to get pregnant on their own and subsequently bear a baby. Its presence increases the likelihood of a transverse arrangement of the fetus. Therefore, in most cases, a caesarean section is required.

The effect of septum on childbirth
The septum in the uterine cavity, even if successfully conceived, can adversely affect the process of the baby being born. Doctors warn of the following problems:
- Premature birth. They begin due to the pressure of the septum on the already large enough fruit.
- Worsening contractility of the uterus. If the fetus is in a transverse position, one part of the uterus and its muscles practically do not stretch during pregnancy. As a result, discoordination or weakness of labor occurs. In rare cases, the intrauterine membrane becomes a cause of a condition dangerous for a woman, when the uterus quickly relaxes after childbirth. This leads to profuse bleeding, stopping which is possible only through resection of the entire genital organ.
Such complications are rare, but they are not excluded. That is why a woman during pregnancy and at the time of birth should be under the close attention of specialists.
Prognosis for recovery
As medical practice shows, the most optimal option for eliminating pathology is hysteroscopy. This is a less traumatic operation, after which no scars remain. In addition, it increases by 70-85% the possibility of childbirth in a natural way.
In some cases, complications arise in the form of infertility. That is why a qualified specialist should deal with the treatment of pathology. It is important for the gynecologist to take into account not only the clinical picture, but also the general state of the patient’s health.