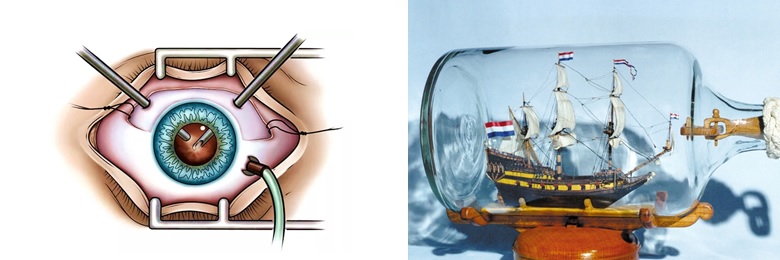
When something enters the ball with the gel, which is the eye - blood cells or inflammation, a foreign body or the structure of the membranes is disturbed, there is a need to work inside the eye in the vitreous body close to the retina. So this is vitrectomy - the work of “cutting” vitreum fibers (vitreum) - the vitreous body, removing it through thin tubes and filling the eye with some kind of medium - water, oil or gas. It looks like an assembly of a 17th century sailboat inside an opaque bottle with a narrow neck. Only the walls of the "bottle" is the retina, which cannot be damaged in any way.
In general, the eye can be pierced in several places with glands, something can be removed inside the cavity and the eye itself can be preserved, and vision can be improved.
How then to live with it and why no one is safe from it - today's post.
Vitrectomy - where we carry out the “haircut”
The eyeball is conditionally divided into two sections - front and back, the diaphragm of the lens and iris serves as the boundary between the sections.
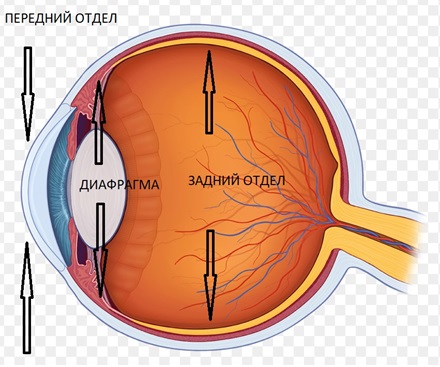
Scheme of the eye
The cavity that is located behind the lens is just filled with a vitreous body lying on the retina. The vitreous itself is a fibrous jelly-like, almost transparent structure. It takes about 2/3 of the volume of the eyeball, provides its volume and tone, as well as shock absorption during shaking. Its structure forms a thin network of interwoven fibers of various forms of collagen protein, surrounded by a dense skeleton, which consists of protein fibrils. Gelatinous and viscous in itself. I wrote about this in detail here: “Flying midges” in the eyes or where “broken pixels” come from in the vitreous . ”

Since the fibers of this vitreous are quite intimately adjacent to the retina, and in some places are attached to it, it’s just impossible to pull these ropes. Simple aspiration as with cataracts (written about it here ) is not enough.
On the contrary - in no case should you pull! The principle of removal is to finely chop and then suck. Therefore, to work in the vitreous cavity, special surgical skills and separate machines for performing vitrectomy are required.
Vitrectomy of the eye can be of two types, depending on the extent to which the vitreous body is removed - in whole or in part: total (almost the entire vitreous) and subtotal or partial (part of the vitreous). Partial vitrectomy, in turn, is divided into anterior and posterior.
An attentive reader will immediately notice: “Where does the vitreous come from in the front segment, which should not be there?”
So in rare cases, the vitreous penetrates through the pupil or other holes into the anterior chamber of the eye. This can happen, for example, after an eye injury, during surgery for cataracts or glaucoma, as a result of problems with the lens of the eye. Since leakage of the vitreous gel can lead to serious problems with the retina, anterior vitrectomy is needed to minimize the risk of complications and help restore vision. The prolapse of the vitreous gel is called a “hernia” and requires removal.
This operation is the most important tool in the surgeon’s skill set, which operates the anterior segment of the eye, but is most often an unplanned and undesirable addition to cataract surgery.

Vitreous hernia
Vitrectomy performed in diseases of the posterior segment is called posterior vitrectomy. This type of surgery is performed by a specialist in retinal surgery.
What can we see in diseases of the vitreous body and in what diseases
Well, of course, most often these are flies (glassy worms) , floating flakes in front of the eyes or general fog, a shroud or curtain in front of the eyes, as well as various artifacts - flashes, lightning, image distortions, broken lines or a black spot in front of the eye, as described here .
And sometimes we don’t see anything — when the problem is on the extreme periphery — then it’s the doctor’s task to look through the pupil into the keyhole and examine the eye from the inside. How this happens is described here .
A huge range of diseases requires such operations - immediately with tomography images:

Central “holes” or macular holes;

Shrinking of the retina due to the appearance of a dense layer of the vitreous body fused with it (the appearance of an epiretinal membrane, epiretinal fibrosis);

Retinal disinsertion;
And also eye diabetes - when tissues with blood vessels, bleeding and wrinkling structures inside, vitreous hemorrhages (for example, due to trauma or hypertension), intraocular infections, retinopathy in premature and quite a few other unpleasant conditions grow into the vitreous body.
Vitrectomy - procedure engineering
The operations on the vitreous body are diverse and complex, high-tech. Why? Because the surgeon works on the retina with a thickness of 100 microns (1/1000 mm), through punctures of 0.5-0.6 mm in size, on a device with complex optics, an integrated laser and a tricky system for maintaining intraocular pressure.
After all, a reasonable question begs itself: if there are at least 3 holes in the eye, then why doesn't it arise? How can you see anything in a small, dark inside ball about 24 mm in size, and even carry out some manipulations for several hours?
The modern principles of vitrectomy were developed by Robert Machemer in 1970. Machemer created the suction device, which was the first vitrectomy device with a closed system, which was necessary to control the level of intraocular pressure during surgery. This achievement was monumental in ophthalmology, as it was the first time to control access to the posterior segment of the eye!
Initially, vitrectomy was used primarily to clean the vitreous body from opacity, such as blood. But the whole operation was so rude that often the severity of the operation was higher than the benefit of the operation itself - the holes for work and the tools were very large - a whole 1 mm! And yes, that’s a lot for the retina!
In modern ophthalmology, technological development and advanced equipment make it possible to use this procedure much more widely.
The surgeon provides access to the patient’s vitreous chamber with stylet with a special sharpening for the correct form of “holes”. To do this, at a distance of 3.5 millimeters from the limb, one sclerotomy opening is made using a puncture, into which the port is then installed, an infusion cannula is placed and two additional punctures are performed - and the ports are inserted through which the vitreotome and the fiber optic tip are inserted (light source )

Vitrectomy - Schematic
All ports have valves that prevent fluid from flowing out of the eye, and a sophisticated system for supplying and controlling the administration of solutions maintains constant pressure inside the eye.
This intervention is now a standard operation for a vitreoretinal surgeon and can be performed on an outpatient basis. Long gone are the days when a 20 gauge vitrectomy was first introduced. Ophthalmologists now have 23, 25 and 27 calibration systems with improved duty cycles and cutting speeds.

This procedure involves the complete or partial removal of the vitreous by cutting and sucking it with tiny ophthalmic instruments that are inserted into the eye. Surgical removal of the vitreous body is necessary for unhindered access to the retina. The surgeon introduces much smaller instruments into the eye and removes cicatricial and pathologically altered tissue, and individual sections are gradually aligned. During surgery, it is often used by a laser to strengthen the retina in the correct position.
A vitreotome or vitrector — like a guillotine knife finely chopping, “shredding” vitreous fiber at a tremendous speed — the standard frequency of operation of a pneumatic or electric vitreotome is 4,000 - 6,000 cuts per minute.
Today I work on a device that has as many as 20,000 cuts per minute and many different tricky modes so that you can safely approach the retina and “shave” and “shave” it as thoroughly as possible. This is one of the most modern cars, damn fast and beautiful - from the Italian car designer of the famous Giorgetto Guigiaro.
Vitrectomy for retinal detachment
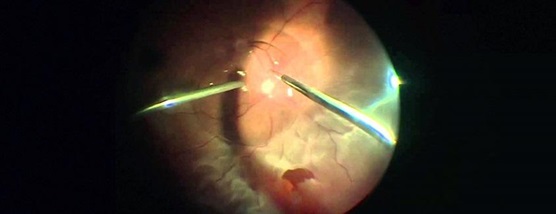
If you illuminate the eye from the inside, then just like that it will be impossible to see anything. Therefore, to obtain an image, complex optical lens systems are used that are built into the heads of modern microscopes, as well as special removable optical systems. They provide an excellent overview, regardless of patient refraction, and allow you to work non-contact and with high magnification.
Optical tomographs are built into ultramodern microscopes to not only see, but also obtain optical media of low-visible structures - all this to increase the accuracy and control of the manual work of a vitreoretinal surgeon.
All work is done through the pupil, so the better it expands, the greater the overview during the operation of the surgeon. The cornea and lens should also be transparent - otherwise the whole picture will be blurred. That is why vitreoretinal surgery is often combined with lens surgery - including to improve the conditions for examination of the fundus. In opaque environments, endoscopes can be used.

Vitrectomy (view from the surgeon)
And the most interesting thing is that the picture that the surgeon sees is turned upside down and does not really exist - this is an imaginary image hanging between the eye and the lens system. Therefore, vitreoretinal surgeons learn to see such images and focus on them, and for the "revolution" of the image, there is an inversion system that connects upon request.
In some cases, when working it is more convenient to work with direct contact lenses mounted directly on the surface of the cornea, for example, when working in the central regions of the cornea - then the image is straight and true.

Work through a contact lens
In most cases, local anesthesia is suitable in combination with special local blockages, but in some cases, anesthesia may be required.
Removal of epiretinal membranes - what is the topic? How and why is it done?
The epiretinal membrane is a conglomerate consisting of vitreous structures, degenerated and fused to the inner layers of the retina. It can be like a blanket on the surface of the retina, wrinkle it, tear and pull, causing delamination. It occurs with inflammation, trauma, exfoliation, aging and other multiple conditions of the eye.
To remove a 3-5 mm thick membrane several microns thick - 70 times thinner than a human hair , the surgeon uses special thin tweezers and manually grabs the membranes (as a rule, pre-staining them with special dyes). If the density of the membranes is high, we use microscissors and other "tenacious" tools. If the membrane “bleeds” - we cauterize and work further, releasing the retina for each millimeter. An analogy with collecting a “sailing ship” inside a bottle is appropriate here.
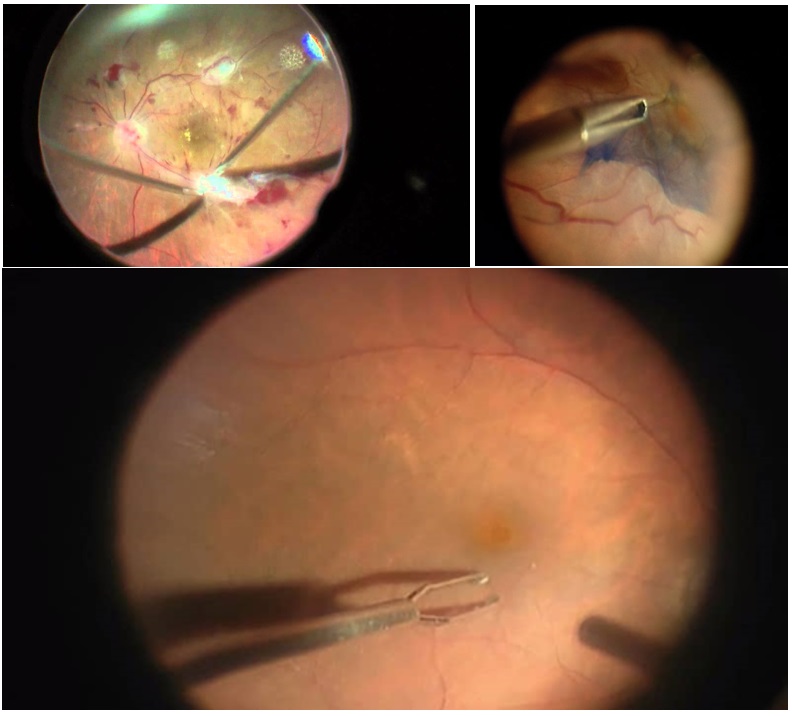
Epiretinal Membrane Removal Options
And will a new vitreous body grow after removal?
The removed vitreous, alas, does not grow back, but is replaced by a liquid that is usually produced by the eye. This gel is very important during the development of the eyes, but is not necessary for their health or focus after birth. So, if necessary, you can part with him without regret. Vitrectomy eliminates all existing scar tissue - this allows you to return the retina to its normal physiological position.
What fills the eye?
The removed vitreous is usually replaced with special substances with certain properties. Among the basic requirements for substitutes for the vitreous it is necessary to highlight: high transparency (through it you need to at least somehow see), stability and durability, a certain degree of viscosity of the substance; lack of toxicity and allergenic effects.
Most often, salt solutions, organofluorine compounds, silicone oil, and artificial polymers are used as a substance replacing the vitreous body. Salt solutions and gases do not need to be removed, they gradually disappear on their own - after a certain time they are replaced by their own intraocular fluid.

Duration of gas in the eye
If a gas bubble was placed in the eye, the surgeon may recommend that the patient keep his head in a special position for some time. With a gas bubble or other substance in the eye, the vision will be blurred and there are certain restrictions: the patient is not recommended to fly on an airplane or travel at high altitudes until the gas bubble disappears.

Sleep position after air-gas tamponade
But silicone in the form of oil requires removal - it will not go anywhere from the eye until you pump it out. The period of use of silicone oil is limited to a certain number of years. With regard to the use of artificial polymers, for example, perfluororganics, their presence in the eye should not exceed 10 days - because they are toxic.
The choice of substitute solution is always at the discretion of the surgeon - everything is very individual. But the general principle is the following according to the “sandwich” principle - perfluors are the heaviest, then heavy silicones (heavier than water), saline solution, then light silicones (float up), then gas-air. And gases, in turn, expand in volume - so you have to figure out what to enter, where, when and in what volume. So, if physics and chemistry weren’t the surgeon’s favorite subjects, he won’t make a quick decision.
What and in what cases is used is listed here: https://habr.com/en/company/klinika_shilovoy/blog/409569/
And yes, after a couple of weeks or months, silicone is removed from the eye with the help of another, another surgical intervention. And for him, again, he needs a complete set of tools that determine the cost. Silicone is removed as soon as the retina heals.

Tools
In modern machines for microinvasive vitrectomy, instruments are sold in disposable sets (hence the high cost of surgery) - these kits are expensive, but it is convenient for the surgeon - all standard instruments are at hand.
The pack includes:
- Pneumatic high-speed vitreotome - is a special cylinder with a knife (it removes the vitreous body slowly and in a controlled manner) - it determines the size of 23-27 G;
- Fiber optic luminaires - can be wide-angle or give focal light. In the surgeon's hand, as a rule, there is one lamp. But if it is "dark" or a second hand is needed, that is, additional suspended self-locking multipoint chandelier lamps (chandeliers) that illuminate the eye from the inside;
- Infusion cannula (infusion port used to replace fluid in the eye with saline and maintain proper eye pressure). A flexible tube about 25 cm long is attached to it; it is attached to the infusion source;
- Valve Ports 23.25 or 27 G

The set does not contain micro tweezers, scissors, scrapers - that small instrument that each surgeon chooses "for himself" depending on his preferences and tasks.
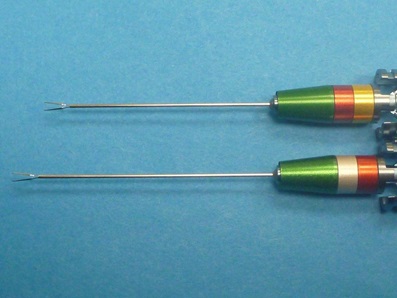
Vitreoretinal tweezers with different working lengths for normal and myopic eyes.
A little bit about the safety of vitrectomy - complications and consequences
Patients may experience mild discomfort for several days after the procedure, the eye may look red, and in general a couple of weeks you may be asked to live upside down. All this for the benefit of the patient!
Although the results of vitrectomy vary depending on the individual condition, most patients experience an improvement in visual acuity after this procedure. However, it is impossible to give guarantees that, for example, the retina will not fall off again - such a risk is always present.
The operation is considered safe in experienced hands, but I do not advise you to fall into inexperienced - you can completely lose your eyesight. But even with an operation ideally performed from a technical point of view, there are certain risks. Some of these include retinal detachment (5.5-10% of cases), the appearance of edema, the growth of new blood vessels, infection (about 0.039-0.07% of cases) and bleeding (hemophthalmus). Cataract formation is often accelerated in those patients who have not previously been operated on to remove it.
The duration of the operation varies from one to several hours, depending on the condition of the patient. I sometimes have patients who have to be operated on for several hours! In certain situations, the doctor may perform another surgery, for example, to remove cataracts.
Vitrectomy in 86% of cases after six months causes cataracts in people over 50 years old, increases the risk of glaucoma 4 times, the risk of retinal detachment 5 times, and can lead to loss of field of vision. Therefore, it is done only according to indications.

WHEN SIZE IS IMPORTANT
And here there is an inverse relationship - the smaller the better (in most cases, but not always).
27 G is less than 23 G, and especially 20 G!

Stylet and vitreotome tips in comparison
Microinvasive closed posterior vitrectomy is less traumatic, significantly reduces the risk of developing intra- and postoperative bleeding, can be performed on an outpatient basis, this does not require hospitalization of the patient. It is usually performed under local anesthesia with sedation (the patient is awake during the procedure, but does not feel pain, but sees the procedure being performed). Significantly reduced the duration of the rehabilitation period.
Present and future - of course, robots
At the European Ophthalmological Congress in Paris this year, the robotic hand of the surgeon is presented - it allows you to reduce tremor and increases accuracy to an incomprehensible height!

The era of digital visualization has come in microsurgery - with the help of 3D systems we can operate, looking not at the microscope’s eyepieces, but at 3D glasses on the display screen - this increases ergonomics and allows to significantly (2.7 times) increase the depth of field of the doctor’s field of view during procedures, as well as volumetric detail for the specialist area of surgical intervention. The complex is used as an addition to a surgical microscope.
The system consists of a high-tech three-dimensional high-definition camera and a station that transmits images directly during the operation or in recording. Thanks to the use of the new system, the overall visualization of the operation process is improved - the doctor sees a three-dimensional image, can, if necessary, enlarge the images on the area of interest, apply filters to highlight certain tissues, and so on. As a result, this is expectedly reflected in the quality of surgical procedures, significantly increases the efficiency and safety of operations, and makes them more comfortable for both the patient and the surgeon himself.
Output
Vitreoretinal surgery is a complex, complex, often multi-stage process that is difficult to standardize. In severe cases, it is a costly surgery lasting up to 2.5-3 hours.
Trust your eyes to professionals. Know that we - vitreoretinal surgeons have super-systems for visualization in the vitreous cavity (microscopes, wide-view systems, illuminators, endoscopes). Chemistry came to the rescue with its materials: perfluors, silicones, gases, and we know how and when to “inflate” the eye safely. To fix the retina there are special lasers and a “freezing” cryo and even “retinal nails”. Modern methods allow in almost all cases to straighten, clean and adapt the retina in any situation - but it is better not to delay it!