Computer technologies in medicine: the history of communication, meaning and prospects. Part I

It's no secret that computer technology has penetrated almost all aspects of modern society: politics, defense, entertainment, education, and much more. Medicine is no exception. Now it is not a secret, but 60 years ago it all seemed like science fiction.
Today we will touch on the past, present and future partnerships of these very different branches of medicine and computer technology. We will find out what revolutionary discoveries have been made, what shortcomings and dangers this partnership carries in it and, finally, what future of medicine awaits us.
The use of computer technology in medicine
At the moment, computers have become widespread in many branches of medicine. Starting from the CPOE (computerized physician order entry) - a computerized physician prescription system (prescribing tests and / or medicines), ending with robots interns that help surgeons during surgeries. Also, computers play no small importance in the work of clinics as a whole, helping to plan and carry out various administrative tasks, keep track of finances, conduct inventories, etc.

The Internet has also played a minor role. Thanks to him, a new direction in medical diagnostics appeared - teleradiology (in other words, transmission of images and data of a medical nature through the world wide web). This innovation made it possible to analyze the patient's data and make decisions regarding his treatment while being away from him, thereby saving valuable time. Also, doctors were able to quickly consult with their colleagues from around the world. A huge base of medical knowledge stored on the Internet is available to patients, giving them the opportunity to get acquainted with their disease, recognize the symptoms, find out the necessary information about the doctor and / or clinic, about drugs, etc. Regarding the use of the Internet patient goes quite a bit of controversy. The fact is that trusting the patient himself to establish a diagnosis and prescribe treatment is extremely dangerous for him. On the other hand, if a patient combines the use of information from the Internet with a visit to a real doctor, this can improve the quality of his treatment.

And perhaps the most unusual use of computer technology in medicine is video games. They are used to train surgeons who will later perform laparoscopic operations (when small cuts are made in the area of the operation for the operation inside, instead of a large incision and an “open” operation). Studies in 2004 showed that surgeons playing video games about 3 hours a week make 37% fewer errors during such operations.
Chronological scale of interrelation of computer technologies and medicine (1954-2006)
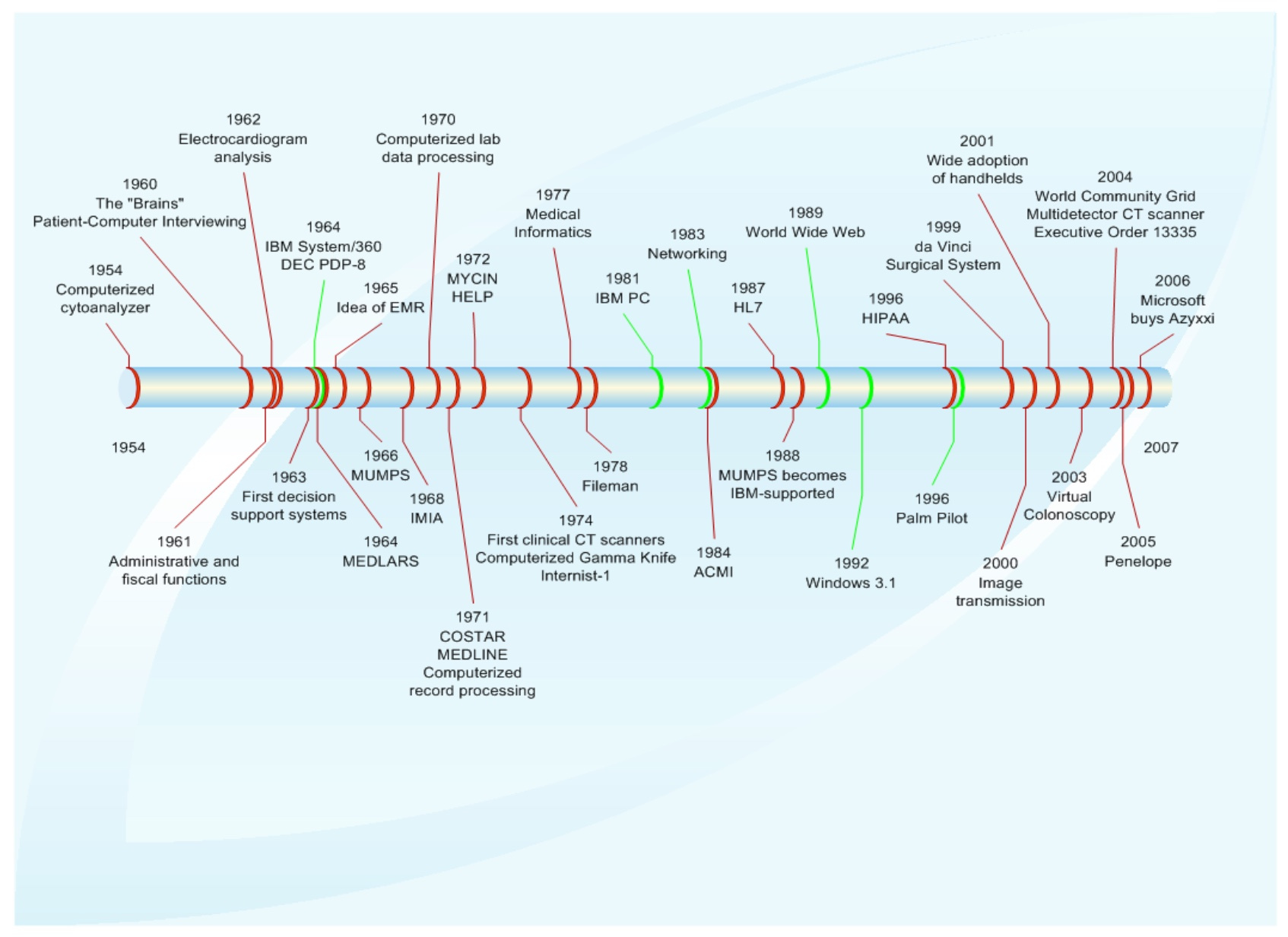
| Year | Event | Description |
|---|---|---|
| 1954 | Computerized Cytoanalyzer | Electronic optical device for screening cells suspected of malignancy. |
| 1960 | “Brains” | The IBM 650 called “Brains” is a scan of medical records to detect subtle anomalies. |
| 1960 | Computer patient survey | Computerized patient history |
| 1961 | Administrative and fiscal functions | Implementing computers to perform administrative and fiscal functions |
| 1962 | Electrocardiogram analysis | Electrical impulses from the heart were transmitted by telephone to the central computer, which created the curve and analyzed it. |
| 1963 | First decision support system | Introduced a computer approach to rehabilitation. For example, a computer was used to determine the optimal time to wear gypsum during surgery. |
| 1964 | IBM System / 360 | The release of computers S / 360 |
| 1964 | DEC PDP-8 | Presentation of the mini PDP-8 computer |
| 1964 | MEDLARS | MEDLARS is a computerized database system for indexing and retrieving medical quotes from the National Library of Medicine (NLM). |
| 1965 | EMR idea | The development of the idea of an electronic medical record |
| 1966 | MUMPS (Massachusetts General Hospital Utility Multi-Programming System) | The Massachusetts General Hospital Multi-Programming System (MUMPS) - also called “M” - was the programming language for the healthcare industry. |
| 1968 | IMIA | The International Medical Informatics Association (IMIA) was established in France. |
| 1970 | Computerization of data processing from laboratories | The use of computers for laboratory calculations, such as the determination of the chemical composition of the amniotic fluid. |
| 1971 | Computerized record processing | IBM System / 3 Model 6 was used to process patient test results. |
| 1971 | COSTAR | Base of outpatient patient records, written in MUMPS |
| 1971 | MEDLINE | MEDLINE went online |
| 1972 | MYCIN | MYCIN is an interactive expert system for the diagnosis and treatment of infectious diseases. Developed at Stanford Medical School based on DEC PDP-10. |
| 1972 | HELP | Health Evaluation through Logical Process (HELP) was developed in the LDS hospital |
| 1974 | CT scan | A CT scanner was invented by Hounsfield and Cormac in 1972 (for the head only). In 1976 - for the whole body. |
| 1974 | Computerized gamma knife | Introduction of the first gamma knife training dose planning computer program (method of radiosurgical removal of brain tumors). |
| 1974 | Internist-1 | Computer diagnostic system developed by the University of Pittsburgh. |
| 1977 | Medical informatics | Defined the term "medical informatics" |
| 1978 | Fileman | A set of utilities written in the MUMPS language that implemented metadata functions. |
| 1981 | Ibm pc | Personal computer from IBM was published |
| 1983 | Network | Networking Public Representation |
| 1984 | ACMI (American College of Medical Informatics) | The American College of Medical Informatics (ACMI) was created. |
| 1987 | HL7 | Health Level Seven, Inc. (HL7) was established as a standard for sharing clinical data. |
| 1988 | MUMPS and IBM | MUMPS becomes language supported by IBM |
| 1989 | WWW (World Wide Web) | The invention of the World Wide Web |
| 1992 | Windows 3.1 | Windows 3.1 release |
| 1996 | Palm pilot | Launch of the Palm Pilot (Pocket PC) |
| 1996 | HIPAA (Health Insurance Portability and Accountability Act) | Congress passed the Portability and Accountability Health Insurance Act. |
| 1999 | Da Vinci Surgical System | This robotic surgical system was developed by Intuitive Surgical. The prototype was introduced in the late 1980s at the Stanford Research Institute under contract with the US Army. |
| 2000 | Image Transfer | The clinics began to transmit electronic copies of diagnostic images (x-rays, MRI scans) |
| 2001 | Widespread PDA | In the early 2000s, healthcare workers widely used handheld devices to perform tasks such as access to medical literature and electronic pharmacopeia. |
| 2003 | Virtual colonoscopy | Virtual colonoscopy uses a combination of CT scan technology and computer graphics. |
| 2004 | WCG | IBM launched this project to search for genetic markers of various diseases. |
| 2004 | Multipoint CT Scanner | This new cardiac scanning technology can largely replace angiograms. |
| 2004 | Decree number 13335 | President Bush issued a decree called "Incentives for the Use of Medical Information Technologies" |
| 2005 | Penlope | A robot intern was introduced to the world. |
| 2006 | Microsoft buys Azyxxi | Microsoft bought clinical medical software that can extract and display various types of patient data. |
Electronic Medical Records (EMR)
Back in 1960, an article was published in the New York Times newspaper in which one doctor from the University of Tulane expressed an interesting thought about "medical records stored on film, or another method suitable for a computer that can completely crowd out written records of patients." In 1967, another article mentioned the following vision of the future - “every man, woman, or child can have all of their medical data electronically recorded in a huge memory system in Washington.” Let's discuss the benefits of such a system. If, for example, a person has a heart attack, and he is in another city. The article responded: “It will be enough for the prescribed doctor to call to Washington, and after a second before him there will be all the data from this patient. Now, more than half a century later, we see how such systems have become a reality and have spread widely in various medical institutions all over the world.

In addition to the advantage of remote data access, the EMR has others that will be discussed later. Based on these advantages and the fact that the idea of electronic recordings has existed for many decades, you might think that EMRs are used absolutely everywhere. However, this is not quite true. For example, in the US, EMR is used only in 17% of clinics.
EMR history
In the late 1960s, a programming language called the Multi-Programming Multi-Programming System (MUMPS) Massachusetts General Hospital Utility Multi-Programming System (MUMPS) was developed for use in healthcare systems. It did not become widespread until the 1970s, when it began to be used to create many clinical programs. To this day, many old systems work with software based on MUMPS. Despite its initially medical direction, MUMPS is widely used in other industries that require a large number of simultaneous connections to the database (banks, stock exchanges, travel agencies).
For acquaintance with the MUMPS language you can follow the link to the pdf-tutorial
In 1978, Joseph (Ted) O'Neill and Marty Johnson, together with their team, developed Fileman using the MUMPS language. Fileman was a set of generalized procedures, specially simplified for users who do not understand MUMPS and programming in general. From the late 1970s to the early 80s, many utilities were designed on the basis of Fileman. Later, the US Department of Veterans Affairs began using Fileman as its official medical program.
In 1981, in Florida, Mickey Singer founded a software company called Personalized Programming Inc., which was one of many that later formed Medical Manager Inc. It provided clinics and private practitioners with software, the popularity of which was so great that by 1997 more than 24,000 clinics and 110,000 practitioners used it. However, only a fall followed. Instead Medical Manager Inc. came the Open Public Public License (GPL), which provides its users with the source code of the software, giving them the opportunity to perform the necessary customization.
Currently, the number of companies providing solutions for EMR varies from 250 to 500. Some of them are focused on small systems, such as prescription or medical history. Others offer package solutions.
EMR benefits
The main EMR users are doctors and other medical personnel. Standard EMR gives them access to the electronic version of the patient's medical history, which had been stored on paper for many years. So why change something that worked so long?
- The answer is simple - doctors' mistakes. One of the main problems of medicine in all epochs was the iatorogenic complications of the patient's condition, that is, those that were unintentionally caused by the actions of honey. the staff. For example, the appointment of the wrong drug or the appointment of too large or small dose. Electronic medical records in conjunction with clinical decision support systems are capable of providing automatic checks to prevent such errors.
- Another advantage already mentioned in this article is access to the database from anywhere in the world. This allows you to better coordinate the work of various specialists, reducing the time taken to review the history and decision making. And time, as we know, is very often a critical factor in the struggle for the life and health of a patient.
- To facilitate the work of doctors and reduce the time spent by the patient to visit them, coordination of EMR with other systems, such as laboratory, is also necessary. Previously, the patient came to the doctor, he assigned him certain tests / tests, the patient went to the laboratory, transferred the appointment, did the tests and the results were recorded on paper again and should have been transferred to the doctor. This is a long process, during which errors and confusion are not uncommon. Let's start with the classics - the doctor's handwriting may be illegible, the wrong tests may be conducted, the results may be lost or confused. If we use the interconnection of two electronic systems, then the direction and results will be placed in the patient's electronic folder, which has access to a doctor.

- This ill-fated medical handwriting carries many problems in the process of extracting drugs. A pharmacist may incorrectly read either the name or the dosage of the medicine, and this, as you understand, can have terrible consequences. Electronic recipe system eliminates the possibility of such a "misunderstanding".
- It is also important convenience for patients, because they do not need to ring up all the clinics that they visited to collect the necessary medical history. All of it is stored in the patient's folder.
- Electronic patient records can (and should) be backed up, etc. make backups. With paper notes, this is difficult, and, in truth, no one did. For example, after Hurricane Katrina, thousands of patient histories were lost, and their recovery took many months.
- The more common the EMR will be in the world, the easier it will be for researchers. A huge database of patients, their symptoms and diseases, treatment methods and the healing process - all this will help to study certain diseases, improving methods of dealing with them.
- In the long run, the use of EMR is cost effective. There is no need to spend money on the office (this is a trifle, but on a global scale, the sums will be large), a reduction in the number of staff, a reduction in time and, consequently, an increase in labor efficiency.
EMR Disadvantages
Despite the very impressive benefits of EMR, their speed of propagation is not impressive. Now we consider why.
- Many modern EMR are incompatible. The fact is that each clinic has its own base, which does not work with the base of other clinics. As it is not profitable to facilitate the process of the patient's transition to competitors, you understand.
- The big issue is always the confidentiality of information. How to make so that only the necessary information fell into the hands of only the right people? How to protect the EMR from hacking? Many do not want to answer these questions simply by refusing to introduce an electronic system.
- In order for the EMR to be complete, it must have a patient history, not just fresh data. Accordingly, this story needs to be added to the base, and this is a lot of manual work, which requires not only time, but also financial costs. At this, many clinics are not ready.
- Now the format in which data is stored alone, but what if in the future it changes? Will it be possible to access the data? Very strange questions, I agree. But they discourage clinics from embracing EMR.
Clinical Decision Support System (CDSS)
In this section, we discuss the history of clinical decision support systems (CDSS), current research, commercial orientation, and potentially interesting areas for future research.

CDSS history
- 1960 - patient-computer
Perhaps one of the earliest uses of computers to support doctors was the computerized patient interview system. The creation of such a system was prompted by the fact that the doctor, when interviewing the patient, often asks the wrong questions or forgets to ask the right ones. Thus, the history will be incomplete, and treatment is less effective. Accordingly, formalized questioning will be much more effective. In 1960, this process was automated using a computer. - 1970 - Expert System
Expert System is a classic example of a decision support system. In the early 70s, research in the field of application of computer technology in medicine was mainly focused on the diagnostic process. It was believed that a computer with a large computing power, can greatly simplify the process of diagnosis. The first such expert was MYCIN, a system developed at Stanford University aimed at diagnosing and treating blood borne diseases. MYCIN proved to be a very accurate diagnostician, making far fewer errors than generalized doctors. However, no one was in a hurry to use MYCIN. There were many different questions and disputes. Doctors did not want to be replaced. Lawyers did not understand who would be responsible for the diagnosis made by the computer. In addition, the establishment of the system was very difficult, long and time-consuming process. Because MYCIN remained in history simply as a very successful experiment.
- 1980s - Real-Time Clinical Decision Aid Technology
One of the most notable implementations of the computer world in the world of medicine is the monitoring system of the heart and brain of the patient. In the 80s, these systems received automatic functions, such as detecting arrhythmias in an electrocardiogram. And in the 90th, these systems began to be replaced on a PC with special software.
- 1995 - PC and Networking in Health
Many clinics have begun using PCs connected by the network to store and transfer data related to administrative tasks. This was an important step for the formation of a modern CDSS system.
- 2000 - our days - Reference databases and portable access
Computer technologies have made reference information available to any doctor or patient. Today, almost everyone has a PC or a handheld device (tablet, smartphone, PDA), which gives him access to the necessary medical information.
Unexpected consequences of health computerization
As we have already understood, the computerization of the medical field is extremely important and must be developed. This process faces many challenges. Not everyone wants to spend money on the introduction of new systems, staff training. Someone is afraid of legal consequences in the case of data exchange between clinics. There is also the issue of confidentiality of information. All of these are factors hindering progress. But there are opinions claiming that this is not worth pushing, as unintended consequences may arise.
Depersonalization
Dr. Gale Thompson, a practitioner since the 60s, said that computerization leads us to forget that there is concern for the patient. Doctors have forgotten how to determine the patient's condition by their pupils, relying more and more on diagrams and graphs on computer monitors. With this opinion fully agree, and Stephen Angelo, a doctor from Connecticut. He told how once the patient monitoring system had “laid down” at his hospital. Doctors were confused, did not know what to do.

Of course, more and more relying on modern technology, we forget about the good old methods. But, if computerization of health care reduces the number of deaths among patients, I’m ready to give up personalization, as such.
Medication errors
Some doctors argue that electronic systems, while helping to reduce the number of errors, but do not eliminate them completely. That's because a person, as a source of error, controls this electronic system.
This is incontestable, but the problem still remains in the human factor, and not in the system as such. To solve this difficulty, it is necessary to pay more attention to the training of med. the staff. If the staff does not know how to use the system, then, of course, all its advantages lose their meaning. As long as there is at least one person in the industry, there will be mistakes.
Invalid information on the Internet
There are many articles about various diseases, drugs, etc. Many of us used similar content for self-diagnostics and even self-treatment. Of course, information is power, but only when it is correct.

A lot of medical information on the world wide web contains errors. And this can lead to the fact that the patient will start the wrong treatment or simply ignore the potentially dangerous disease. This problem can be solved only by introducing standards for the accuracy of information and methods for its verification and control of publications.
Search for relevant information
Storing the entire patient history in one electronic folder allows the doctor to quickly access it. But is he able to quickly find what he needs in this particular case? The huge flow of information that is necessary not only to see, but also to analyze, may delay the formation of history and diagnosis.
Conclusion
The world does not stand still. Computer technology more and more crashes into other areas of our life, introducing many new, good or bad, it is sometimes difficult to say. But progress cannot be stopped, relying only on the fear of something new. This also applies to medicine. Many diseases would remain incurable if some brave souls did not decide to treat them differently, not like before. The main thing to remember is that man creates technology, man improves it and only he can be responsible for it.
Today, many clinics are moving to remote storage and processing of information. We also offer solutions for this type of customers, even solutions using the latest NVMe drives, which allow processing requests in large databases “instantly”. The data centers where the equipment is located correspond to the required levels of certification in the field of data security. And the geographical distribution and isolation of modules, even within the same location, allows you to organize the most fail-safe systems for clients of this kind.
As advertising. Stock! Only now get up to 4 months of free use of VPS (KVM) with dedicated drives in the Netherlands and the USA (configurations from VPS (KVM) - E5-2650v4 (6 Cores) / 10GB DDR4 / 240GB SSD or 4TB HDD / 1Gbps 10TB - $ 29 / month and above, options with RAID1 and RAID10 are available) , a full-fledged analogue of dedicated servers, when ordering for a period of 1-12 months, the conditions of the promotion are here, existing subscribers can receive a 2-month bonus!
How to build the infrastructure of the building. class c using servers Dell R730xd E5-2650 v4 worth 9000 euros for a penny?
All Articles