Polyp of the uterus is a very common, prone to renewal disease. Recurrent endometrial hyperplasia in 1.5% of cases malignant. The greatest likelihood of developing cancer of the uterine mucosa is associated with adenomatous polyps (adenomas). The disease can develop at any age. The optimal treatment method is hysteroscopy (removal of the endometrial polyp). The operation is minimally invasive and high-tech, which significantly reduces the likelihood of the resumption of pathology and the development of negative consequences.
What is a uterine polyp?
A pathological formation that rises above the surface of the endometrium (mucous membrane) of the smooth muscle genital organ in which the fetus is born is called a uterine polyp in medicine. They have a different configuration, consistency, narrow or wide base, smooth, villous or lobed surface. The sizes of neoplasias can be different: from sesame seeds to a golf ball. Polyps of the uterine mucosa are single and multiple. The term "polyposis" is used if the number of neoplasias is more than twenty.
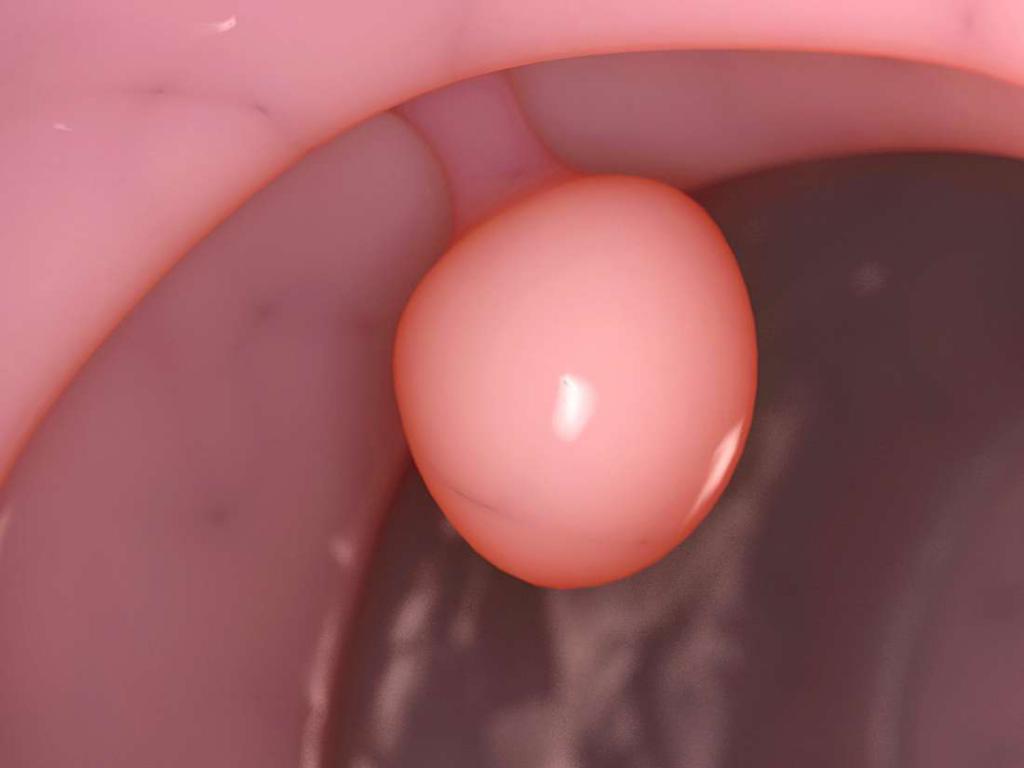
In its structure, the polyp consists of three components. The surface of the formation is covered with epithelial tissue, the leg consists of a fibrous base and thick vessels. Neoplasia can ulcerate, become infected, cell metaplasia, necrotize.
Polyps are most often classified according to their morphological structure. The following types of pathological formations are distinguished:
- Glandular polyps are composed of endometrial tissue containing glands.
- Glandular-fibrous are represented by a mucous layer lining the cavity of the internal genital organ and connective tissue (stroma).
- Fibrous are formed by dense connective tissue.
- Adenomatous polyps are represented by glandular epithelium and are prone to transition to endometrial cancer.
Endometrioid polyps rarely grow outside the uterine cavity. They are detected both in young girls and in women of menopause. In gynecology, the condition is regarded as precancerous, and in most cases an operation to remove the endometrial polyp is prescribed as therapy.
Treatment methods
According to statistics, pathological formations of the uterus are most often formed against a background of a disorder in the hormonal function of the ovaries and an increase in estrogen levels. But hormone therapy is rarely used as the main treatment.

The best treatment method is hysteroscopy - resection of the uterine polyp using endoscopic equipment. Formations on the leg are “unscrewed”, and the bed is cauterized by the cryogenic method or electrocoagulation. Eliminated neoplasia is subsequently sent for histological examination, the results of which determine the further therapeutic tactics.
Removal of the endometrial fibrous polyp is carried out by polyectomy with curettage (curettage) of the uterus. When resecting glandular pathological formations, additional hormone therapy is required. Radical methods of treatment (supravaginal amputation, panhisterectomy) are used to treat uterine adenomatous polyps .
The benefits of hysteroscopy
The use of modern equipment during the operation improves its quality and reduces the risk of complications. In surgery, such treatment methods are quite common. The terminology of the operation, as a rule, comes from the name of the equipment with which it is performed.
Hysteroscopy of the endometrial polyp is the removal of focal uterine hyperplasia using a special endoscopic device in the form of a tube with a fiber optic system and backlight. The operation is endovision, that is, it does not involve opening the cavity. But this is not the only plus of hysteroscopy.
- Surgical manipulation does not require special preparatory measures.
- Resection of focal uterine hyperplasia using endoscopic equipment is less traumatic than classical curettage.
- The negative effects of hysteroscopy (removal of the endometrial polyp) are rarely detected.
- Short rehabilitation period.
- Due to visual inspection, the probability of incomplete removal of the polyp is minimal.
- After hysteroresectoscopy, the neoplasia bed is cauterized, which reduces the number of relapses.
- If the manipulation is carried out using a rigid hysteroscope, it is allowed to use different channels for irrigation (long-term irrigation of the cavity) and aspiration. An operation using such equipment has a lower cost.
Endometrial polyp removal (hysteroresectoscopy): indications
The operation, although minimally invasive, is nevertheless a surgical intervention. The decision to carry it out is made after numerous examinations. Pathologies that are indications for hysterectectoscopy can only be established by a doctor. These include:
- Multiple endometrial hyperplasia, which are common (uterine polyposis).
- Any single polyps that are asymptomatic.
- Endometrial neoplasia of any size, accompanied by regular uterine bleeding.
- The development of anemia caused by frequent secretion of blood from the genitals.
- Abundant vaginal discharge, accompanied by severe pain.
- Menstrual irregularities.
- Inefficiency or complications after curettage.
- Adenomatous (glandular) polyps. Such neoplasms have a high probability of degeneration from a benign to a malignant tumor.
- The threat of spontaneous abortion.
- Hormonal disbalance. Disruptions in the hormonal background can trigger the growth of tumors.

Removal of the endometrial polyp in the uterus during pregnancy planning is carried out to create good conditions for implantation of the embryo.
Contraindications
Before prescribing a resection, the doctor during a physical examination and during the examination identifies all pathologies that impede the use of this treatment method. The general list of health conditions in which the operation is temporarily or permanently not shown is consistent with contraindications to classical ectosomatic surgery.
- Acute respiratory infections (flu, tonsillitis, pneumonia).
- Infectious kidney disease of bacterial etiology.
- Respiratory failure.
- Decompensated heart failure.
- Chronic renal failure.
- Impaired liver function, accompanied by metabolic disorders, intoxication, the development of hepatic coma.
- Shock state.
- Disorders of the hemostatic system.
Contraindications to the removal of endometrial uterine polyps from the reproductive system are:
- Acute inflammatory diseases of the genital organs (vulvitis, cervicitis, salpingo-oophoritis and others).
- Bacterial vaginosis.
- IV degree of purity of the vagina.
- Malignant neoplasms of the uterine mucosa.
- Uterine fibroids are large.
- Submucous fibroids are more than 5 cm in diameter.
For treatable diseases, surgery is delayed until complete recovery. In severe protracted pathologies, treatment tactics are set personally.
Preparation for surgery
Surgical intervention is a very important stage in the treatment of the patient. All manipulations are carried out only with the consent of the patient. Resection of neoplasia of the uterine mucosa refers to planned surgical interventions. Special preparation for surgery to remove the endometrial polyp (hysteroscopy) is not required. Laboratory tests and instrumental examinations are standard for most invasive procedures.
- Examination of a gynecologist on an armchair.
- Bimanual (two-handed) research.
- Diagnosis of the vaginal cervix using a colposcope.
- Smears for vaginal cleanliness and cytology.
- Transabdominal scan of the pelvic organs.
- Clinical blood test.
- Blood biochemistry (glucose).
- A blood test for antibodies to the surface antigen of hepatitis B virus.
- Antibodies to hepatitis C.
- HIV antibody screening.
- Wassermann reaction (RW) - rapid test for syphilis.
- Fluorography.
- Electrocardiogram with decoding.
Hysteroresectoscopy is performed on the 5-15th day of the menstrual cycle. Patients taking synthetic analogues of estrogen and progesterone can be operated on any day of the cycle.
In the morning before polypectomy, standard hygiene and depilation of the intimate area are performed. It is necessary to refuse food intake. The operation is carried out after cleansing the intestine by enema and with an empty bladder.
Hysteroscopy technique
Surgical manipulation is performed using a mono - or bipolar hysteroresectoscope. This is a complex instrument consisting of optics that allows visual control over the process and surgical device.

Removal of the endometrial polyp (hysteroscopy) is performed under intravenous analgesia. The external genitalia, vagina and cervix are treated with an antiseptic solution. The lower segment of the uterus is fixed with bullet forceps. Using the uterine umbrella, examine the depth, position and condition of the uterine cavity. An expansion of the cervical canal is performed for free insertion of an endoscopic instrument. The uterine cavity is filled with gas or liquid. This provides ample space for actions with tools and visual control over the progress of the operation.
A resectoscope and a video camera are introduced into the uterine cavity, which transmits the image to the monitor screen. The doctor examines the uterus, evaluates the condition of the mucous membrane (endometrium), determines the location of pathological neoplasms. Resection of polyps is carried out by an endoscopist.
Single polyps with a clearly visible leg are removed using endosurgical scissors or a special loop. The loop electrode is often used to eliminate large neoplasias located near the uterine wall or having a fibrous structure. To prevent bleeding and reduce the likelihood of resuming the disease, the bed of formations is burned.
After removal of the endometrial polyp, a specialist removes the entire instrument from the uterine cavity and removes gas or liquid. The average duration of the operation is 20-40 minutes. With multiple polyps, technical difficulties, the operation lasts longer. The duration of anesthesia can also be increased.
After operation
After surgery, the patient is transferred to the ward. If the removal of the endometrial polyp has passed without complications, the patient is allowed to go home a few hours after she departs from anesthesia.

In the postoperative period, a course of antibiotics is prescribed for the prevention of infectious diseases. In the early days, a woman may experience aching pain. To eliminate them, the doctor prescribes drugs that stop the pain syndrome.
After the operation, the woman normally has scanty spotting. Usually they pass on their own within 3-5 days.
The removed polyps are sent for histological examination. The results are usually ready in a week, then the patient needs to visit a gynecologist to determine the subsequent therapeutic tactics. After removal of the glandular polyp of the endometrium, treatment with hormonal drugs is prescribed without fail.
Recovery period
The rehabilitation period for each woman goes differently. It all depends on the severity of the pathology, the presence of concomitant diseases, the age of the patient, the quality of the operation.
In the first few days, a slight increase in temperature is possible. The healing process may be accompanied by rare spasmodic pains. Their duration depends on the characteristics of the body. In order for the recovery period after removal of the endometrial polyp (hysteroscopy) to go smoothly, certain recommendations should be observed.
- Do not take baths for 2 weeks after surgery.
- Intensive warming should be discarded.
- Temporarily cancel or reschedule some physiotherapeutic procedures (electrophoresis, laser therapy).
- It is forbidden to swim in pools and ponds.
- Exclude physical activity and sports.
- Do not douche and apply vaginal suppositories without the appointment of a gynecologist.
- The use of vaginal tampons should be discarded.
- Within 3-4 weeks, you must refrain from sexual activity.
Possible complications
Intraoperative complications are extremely rare. The probability of their occurrence is low, but not completely excluded. The list of undesirable situations includes:
- Bleeding. To stop diffuse bleeding, electrocoagulation of damaged endometrial vessels is used.
- Perforation of the uterus due to mechanical damage (trauma to the probe, curette).
- Traumatic injuries as a result of heat and power exposure.
- Weights associated with the use of stretching the uterine cavity.
Complications can occur not only during the operation, but also after it. The negative consequences of hysteroscopy (removal of the endometrial polyp) can manifest itself in the form of the following pathological conditions:
- Accumulation of blood in the uterine cavity.
- Inflammation of the inner lining of the uterus.
- Infection The frequency of occurrence of such complications does not exceed 0.17-3%. The most common are sepsis, bacterial shock.
- Abundant prolonged discharge after removal of the endometrial polyp by hysteroscopy, as a rule, occurs due to non-compliance with medical prescriptions.
- Infertility. Total ablation of the mucous membrane of the uterus can cause the development of inability to conceive or terminate a pregnancy.
- Cervical stenosis. Anatomical narrowing most often occurs after electro- or laser-coagulation of the mucous membrane of the cervical canal.
Treatment after removal of the endometrial polyp
In some cases, the doctor may prescribe additional medication. Medicines are not always prescribed, it all depends on the type of neoplasm. Basically, treatment is prescribed after removal of the glandular polyp of the endometrium. This type of neoplasia is most often observed at a young age. Hormone therapy is aimed at the full restoration of the reproductive function of women.

The selection of hormonal contraception is carried out by the doctor. The combination of “Ethinyl estradiol” (estrogen hormone) with “Dienogest” (suppresses the trophic effect of estrogen) or “Desogestrel” is considered the most effective. The course of treatment can be from 3 to 6 months.
Also, to normalize hormonal processes, an intrauterine device Mirena or James is installed. The active substance of the contraceptive levonorgestrel, causing a decrease in the implantation function of the endometrium. The spiral is set for 5 years.
If a histological examination revealed additional pathologies, then treatment will be prescribed depending on the type of disease. If malignant cells are found in polyps, an additional comprehensive examination will be prescribed and, most likely, more radical treatment will be carried out.
Reviews
Most women are satisfied with how the operation went. They note the convenience that a few hours after surgery, you can go home.
Most often, patients in reviews of the consequences of hysteroscopy (removal of the endometrial polyp) write about prolonged bleeding that opened a few days after the resection. But after taking medication, everything is quickly restored. But in general, women respond positively, especially those who were prescribed conservative treatment, which turned out to be ineffective.
Many patients note the high cost of the operation, but they themselves say that the end result is worth it. After hysteroscopy, doctors often prescribe a course of oral contraceptives. Women who have not previously used such drugs, note the presence of side effects and too long a course.
Pregnancy after hysteroscopy
Infertility after removal of a pathological neoplasm of the uterine endometrium develops only if the operation was performed with a severe degree of the disease or if the woman had problems with conceiving or bearing a pregnancy before.

In reviews of hysteroscopy (removal of the endometrial polyp), young women say that they became pregnant very quickly, and the whole period went off normally. , 3-4 . , , .
– . , .