Cervical intraepithelial neoplasia is most often called gynecological dysplasia among specialists in the field of gynecology. This pathology of the stratified squamous epithelium is regarded as a precancerous condition, where the risk of cell changes is high. At the same time, the disease is treatable.
In most cases, the female body independently cope with the disease in the absence of therapy. But the likelihood of disease progression is not excluded, which, in fact, leads to the development of the oncological process.
general information
What is this type of pathology of the female body and what is the danger? Until 1975, the disease had an excellent name - dysplasia. With the development of the pathological process, the characteristics of mitosis of the cell nucleus and epithelial cytoplasm undergo significant changes. At the same time, the membrane and its upper layers remain intact.
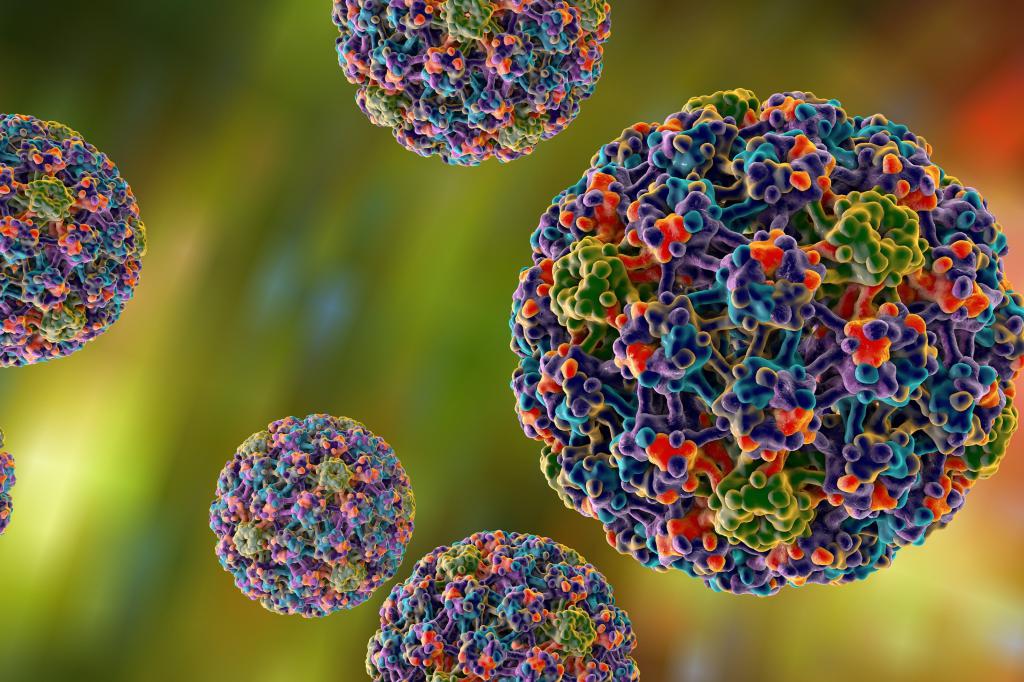
Under certain circumstances, cervical intraepithelial neoplasia is converted to a malignant neoplasm. And if timely treatment therapy is not started, the further development of the disease poses a serious threat to life. The precancerous condition is caused by the activation of the human papillomavirus (HPV) , which is present in the body of almost every person. In this case, experts identify several varieties of the virus, which further exacerbates the situation.
Many people often confuse the two concepts, calling dysplasia erosion. But this is not entirely true, since the last term does not fully convey the essence of what is happening. The fact is that erosion occurs due to damage to tissues of a mechanical nature, and dysplasia is already a violation of their cellular structure.
Every year, around 40 million women are diagnosed with cervical intraepithelial neoplasia of the cervix uteri, which makes up 15 to 18 percent of all cases of reproductive organ pathologies. However, in most cases, young girls aged 25-35 years are at risk. The ratio of incidence is an average of two people per one thousand of the population.
How the cervix is arranged
In order to clearly understand and realize the whole danger of pathology, it is worthwhile to understand the anatomy of the female body, in particular the cervix, well. This term is called the lower part of the genital organ of a narrow and cylindrical shape. Partially, it is located in the abdominal region and slightly enters the vaginal area, in other words, it is located in both areas.
Gynecologists use special mirrors to examine the vaginal part. In the inner part of the neck there is a narrow cervical canal 10-15 mm long. The external pharynx passes directly into the vagina, while the internal pharynx is turned into the uterine cavity. In other words, this is a kind of small tunnel that connects the vagina to the genital organ. Gynecologists use special mirrors to examine the vaginal part in order to detect cervical intraepithelial neoplasia of the cervix.
The cervical canal is covered with cylindrical epithelial cells of a bright red color. Inside them are special glands that secrete mucus, which serves as a defense against various pathogens.
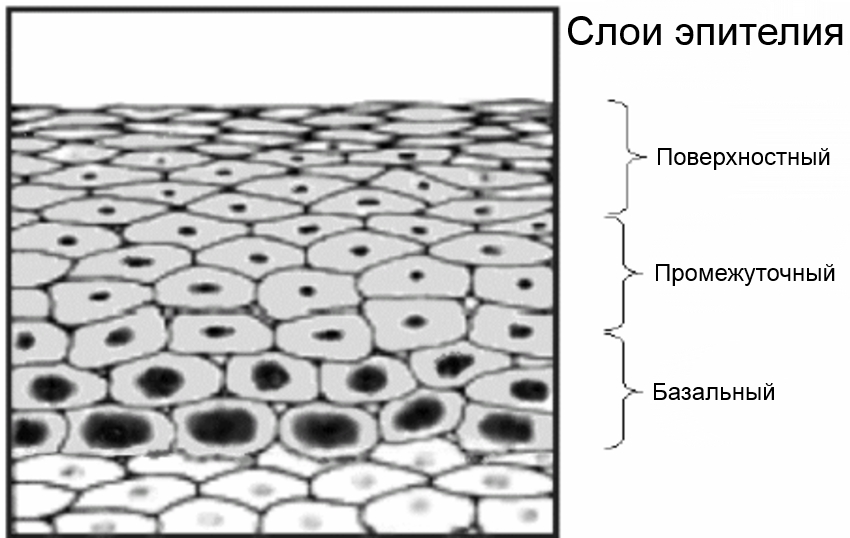
In the region of the external uterine throat, cylindrical cells are replaced by flat ones. There are no glands here, and the shade is already pinkish. Moreover, this epithelium is formed by several layers:
- Basal-parabasal - the lowest border, formed, in turn, by basal and parabasal cells. Under the basal tissue is the muscle structure, blood vessels, nerve endings. There are also young cells that can divide.
- Intermediate.
- Superficial (functional).
Healthy basal cells have a rounded shape, inside them is a large nucleus. Ripening gradually, they rise to the upper layer. At the same time, their shape is flattened, while the nuclei are reduced in size. When cells get to the upper layer, they become flatter with small nuclei.
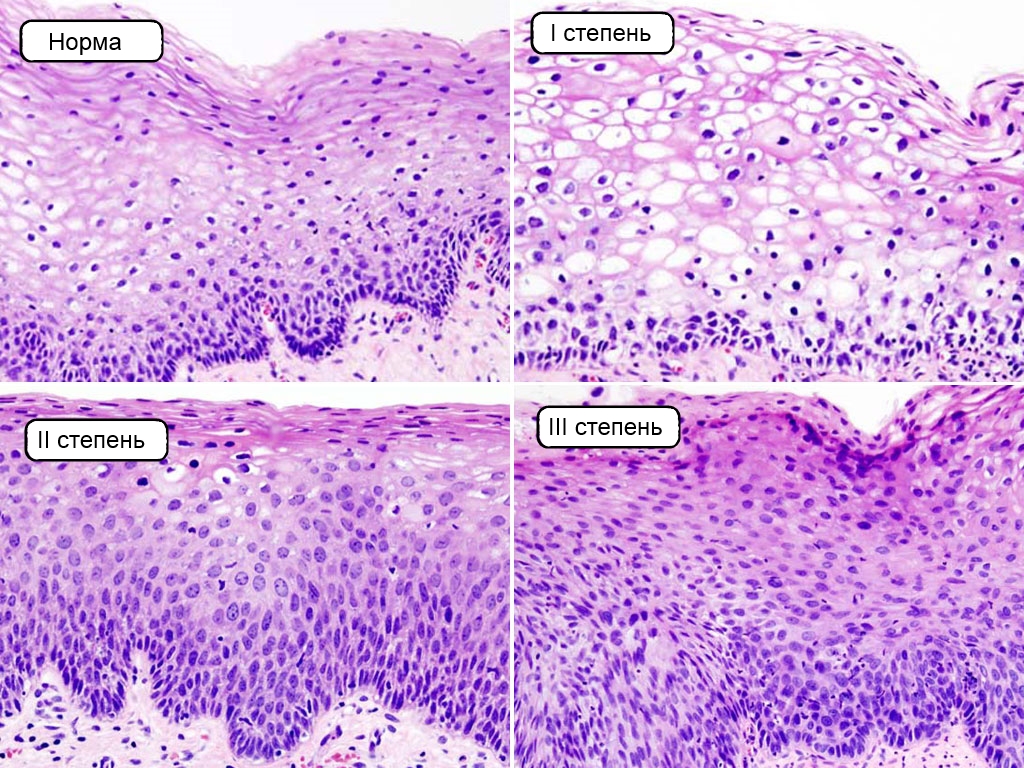
With degree 1, 2, 3 cervical intraepithelial neoplasia, the structure of the cells is already slightly different - atypical elements appear that do not have any particular shape, and their size is very large. In addition, each such cell has several nuclei, and their division occurs even faster.
In the case of a pathological process, different layers of the epithelium are affected, except for the superficial. Altered cells actively grow, and against this background, signs of nuclear atypia form.
Pathology classification
Neoplasia is classified into several degrees, depending on the severity of the pathology and the number of integument epithelial cells involved:
- I degree - easy (CIN1).
- II degree - moderate (CIN2).
- Grade III - Severe (CIN3).
On the territory of the Russian Federation, doctors mainly use this classification by I. A. Yakovleva and B. G. Kukute, 1977.
Mild neoplasia
This is a weak cervical intraepithelial neoplasia, in which the structure of the tissues is slightly changed, there are coil cells. A mild degree of growth of basal cells is also observed. The pathological process affects no more than a third of the thickness of the epithelium.
Moderate dysplasia
Here we are talking about a more pronounced pathological process, which already covers up to 2/3 of the thickness of the mucous membrane of the cervix. Atypical cells are present on the lower and middle layers of the epithelium.
Hard case
In this case, almost the entire thickness of the epithelium is affected. In this case, a clear separation into layers is no longer traced. In addition, pathological changes in mitosis and acanthosis can be detected.
Causes of occurrence
In order for HPV to lead to the development of the oncological process, a number of factors are required. It is worth noting that this virus is not in every woman that can provoke the appearance of cervical intraepithelial neoplasia of the 1st degree. As a rule, from the moment of infection with HPV or its activation and ending with the appearance of a precancerous condition, it takes about 1.5 to 5 years. The oncological process itself is formed over the years or decades.
As for the development of neoplasia of the neck of the genital organ, the appearance of the pathology is caused not by one, but by several factors, as in the case of any other precancerous condition. Here we are talking about a whole combination of provoking reasons:
- Infection with a specific variety of HPV.
- The use of hormonal contraceptives for a long period of time (5 years or more).
- The beginning of early sexual activity (14-15 years).
- Proximity with many partners.
- The presence of bad habits (smoking, not only active, but also passive).
- Weak immunity.
- Surgical interventions and abortions, more than once.
- Imbalance in hormonal balance.
- Sexual diseases of an infectious nature.
- Hereditary predisposition.
But as already noted above, often the appearance of cervical intraepithelial neoplasia provokes precisely the papilloma virus. Moreover, the disease can begin to develop with the absence of symptoms and, as a rule, up to 10 years elapse from the onset of dysplasia to the onset of cancer.
Every person is susceptible to the infection of this virus, but this is especially true for those women who have an active sex life with several partners. A neglect of contraceptives, as well as ignoring the treatment of inflammatory processes of the organs of the reproductive system - all this only increases the risks of developing pathology. In addition, frequent childbirth or abortion leads to injuries of the cervix.
Symptomatology
The danger of cervical intraepithelial neoplasia of degree 2 or more severe is that in most cases a woman simply does not feel the characteristic signs of the onset of pathological changes in the epithelium. At the same time, a woman does not feel pain, there is no increase in body temperature either, nor does deterioration.
Symptoms if they appear, then this will already indicate the presence of an adjunct infection, which leads to the development of a number of diseases:
- Inflammation of the cervix (cervicitis).
- The inflammatory process of the genitourinary system due to exposure to Trichomonas (trichomoniasis).
- Inflammation of the vagina (colpitis).
In this case, the woman will feel itching and burning in the vagina, spotting after intercourse, douching or the use of tampons. Leucorrhoea can also change the texture, smell and color (thick, plentiful and smell bad). With severe cervical intraepithelial neoplasia, pain in the uterine region of a pulling character may occur.

A regular gynecological examination of women using instrumental, laboratory and clinical studies will allow timely detection of pathology and start treatment.
Diagnosis
As we now know, under certain circumstances, neoplasia threatens to progress to the development of a cancerous tumor. For this reason, early diagnosis will avoid serious complications. Any woman over the age of 21 needs to visit a gynecologist every year for a routine examination, and undergo a cytological examination every three years.
Effective diagnostic techniques:
- Gynecological examination.
- Colposcopy.
- A targeted biopsy.
- Histology of a biopsy specimen.
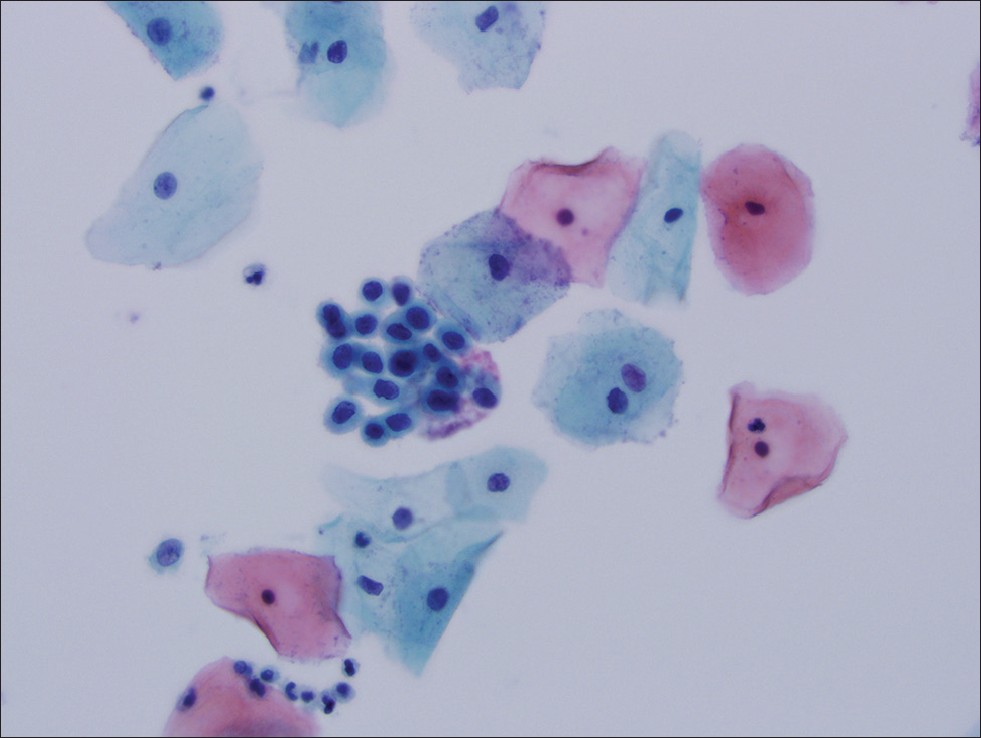
- Pap smear cytology.
The purpose of a gynecological examination is to identify visually visible changes in the mucous membrane. Moreover, in rare cases (3-4%), such an examination does not give the proper result. But mainly in women (20-24%), signs of cervical intraepithelial neoplasia of the 1st degree in the face of a retention cyst, focal or diffuse hyperemia of the mucous neck can be detected. In severe forms of pathology, often (64–73%) characteristic features are revealed: erosion, pseudo-erosion, leukoplakia of varying degrees of keratinization, exophytic growths of the epithelium.
Colposcopy is carried out by a special optical device (colposcope), which is capable of magnifying objects 10 or more times. With it, you can not only carry out diagnostics, but also perform tests. That is, to treat the neck of the genital organ with a solution of Lugol or acetic acid.
A targeted biopsy is performed during the colposcopy procedure. In this case, a sample is taken by cutting off a piece of tissue in the problem area.
Histology of the biopsy is a histological examination of a sample taken during a biopsy. This technique is considered the most effective in detecting pathology.
A Pap smear is examined under a microscope, where atypical cells can be detected, as well as HPV markers, which indicates degree 2 cervical intraepithelial neoplasia.
In addition, an obligatory ultrasound of the genitals of a woman is performed. And as additional measures, a PCR study and a blood test for immune status are proposed.
Treatment methods
The choice of treatment depends on several factors:
- patient age;
- severity of pathology;
- what is the affected area;
- are there any concomitant diseases;
- the presence of allergic manifestations to medications.
If the pathology is poorly expressed, then dynamic observations are performed, and if any infection is detected, special therapy is prescribed. It is worth noting that the treatment of the initial stage of neoplasia is carried out using medications, however, only surgical intervention is indicated in the diagnosis of cervical intraepithelial neoplasia of 2 and 3 severity.
Use of medicines
Since the treatment of neoplasia is carried out mainly through surgical intervention, the use of medicines is carried out as an adjunct therapy.
This is mainly due to the fact that at the initial stage of the development of pathology, there are no characteristic signs. The task of medicines in this case is as follows:
- Increase immunity.
- Normalize the vaginal microflora.
- Elimination of hormonal imbalance.
- Suppression of HPV activity in the body.
- Therapy for sexually transmitted infections (STIs).
As for the medicines themselves, the doctor usually prescribes Interferon, Prodigiosan, Cycloferon, Groprinosin, Kagocel, Genferon and a number of other drugs. If we take into account one feature of HPV, which is to suppress the production of own interferon by leukocytes, and significantly, then the choice of these medications for the treatment of cervical intraepithelial neoplasia (CIN 1) is quite justified.
As an antiviral agent, Panavir is distinguished by good effectiveness. Normalize the vaginal flora with probiotics with bifidobacteria and lactobacilli. STI therapy is carried out with the use of antibiotics, based on a variety of pathogenic microorganism. In addition, the intake of B vitamins, antioxidants, omega acids is prescribed.
At the same time, it is not always possible to completely defeat the pathology, and for this reason, in most cases, doctors still refer patients for surgery. Only before and after such a procedure is a supportive course of therapy using medicines required.
Surgery
Depending on the individual characteristics of the female body, the list of contraindications, the size of the affected area, the prescribed surgical intervention can be of various types.
- Laser excision. This method of treatment of cervical intraepithelial neoplasia of the 3rd degree is carried out using a laser scalpel, which actually excised the affected tissue.
- Radio wave therapy. It is considered a new technique in which the affected area is removed by exposure to high frequency radio waves. For the operation, the Surgitron apparatus is involved.
- Electroconization. Here, the procedure is performed using a metal loop where electric current is supplied. In this case, the affected cone-shaped area of the affected tissue with the inclusion of healthy tissue is removed. The operation is widely used in the treatment of cervical neoplasia. It can also be carried out by the laser method, which manages to minimize the risks of bleeding. The operation is performed after menstruation.
- Photodynamic therapy. It is also a modern way of treating neoplasia. The technique works as follows: after the introduction of a photosensitizer into the body, it begins to accumulate in the neoplasm. In this case, singlet oxygen is released in tissues with a changed structure, which leads to the death of atypical cells.
- Diathermocoagulation and cryodestruction. These methods of temperature exposure in relation to cervical intraepithelial neoplasia of the 3rd degree are used in extremely rare cases, due to the lack of control of the depth and volume of exposure by the doctor. And therefore, the appearance of relapse in this case can not be avoided. Usually, cauterization or freezing applies only to background pathologies, but not precancerous.
Based on the data obtained from the histological examination, the specialist is already making further decisions. If cancer cells are detected, an additional operation or radiotherapy, chemotherapy, is likely to be required.
Possible consequences
Proper treatment of neoplasia of the initial degree contributes to the suppression of HPV replication, resulting in recovery. However, the lack of proper treatment threatens to develop serious complications. Uncontrolled progression of the pathology only aggravates its course, and the transition time of stage I or II of the pathology to cervical intraepithelial neoplasia of the 3rd degree of the cervix depends on the individual characteristics of a person, his local and general immunity.
A moderate stage of the pathology is also still being treated, only in this case the course will be longer, and the operation can often be performed more than once. The most severe degree of neoplasia can form in an oncological neoplasm with a probability of 50%.
However, the most threatening complication is the formation of an invasive form of cancer. At the initial stage, the process looks harmless. On the mucous membrane, this manifests itself in the form of redness. And often during a more detailed diagnosis, chaotic cell division of the epithelium is determined. And if you allow this process to develop quietly, a small tumor is subsequently formed, which then does not prevent anything from increasing, which leads to the spread of metastases.

This can happen after severe cervical intraepithelial neoplasia in case of late diagnosis or when treatment is ignored for any reason.
Pathology and pregnancy
With neoplasia of the neck of the childbearing organ, this is not a contraindication to prolong pregnancy, but at the same time, the course of the atypical process is noticeably aggravated. During the period of gestation, treatment is more important than ever, because when HPV is activated, the microorganism can reach the fetus due to a decrease in the immunity of the female body, which leads to intrauterine infection.
In addition, almost all types of the virus subsequently contribute to the defeat of the larynx of the child. During childbirth, the risk of getting HPV into the respiratory tract of a child is not excluded, which causes a respiratory disease such as papillomatosis.
Alternative technique
We all know how effective folk recipes are for treating various diseases. Cervical neoplasia is no exception, but it is better to get advice from your doctor before conducting such therapy. It is only worth considering that, as in the case of the use of medicines, the treatment of high severity cervical intraepithelial neoplasia is ineffective, and sometimes even pointless.
You can fight pathology with the help of an infusion from the collection of certain types of herbs. To prepare it, take 1 tsp. sweet clover, 2 tsp. yarrow, 3 tsp nettles, the same number of rose hips, 4 tsp each. marigold and meadowsweet flowers. All ingredients mix well, after which 1 tbsp. l pour the mixture with a glass of boiling water and let it brew for 30 minutes. Using this infusion, do douching in the mornings and evenings, and as a supplement, swabs from 30 to 40 minutes soaked in the same solution should be inserted into the vagina. Perform manipulations for a month.

Sea buckthorn oil is no less effective. They should also soak a swab and put in overnight for 60-90 days. Also for these purposes, you can use aloe juice, only in this case you need to use tampons twice a day, and the course is 1 month.